St George's history
View all Close all
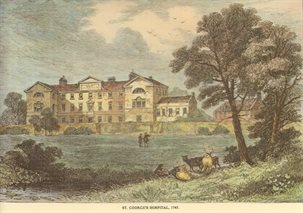
St George's Hospital opened in 1733 at Lanesborough House, Hyde Park Corner in London, in what was then a countryside location. The hospital owes its existence to four men, Henry Hoare, William Wogan, Robert Witham and the Reverend Patrick Cockburn, who collectively founded the Westminster Public Infirmary in Petty France in 1720. The ever-increasing needs of the sick forced the Westminster Public Infirmary to seek improved and enlarged premises. A disagreement between members of both the Governors and medical staff on the choice of building led to the founding of both Westminster Hospital in Castle Lane and St George's Hospital on Hyde Park Corner.
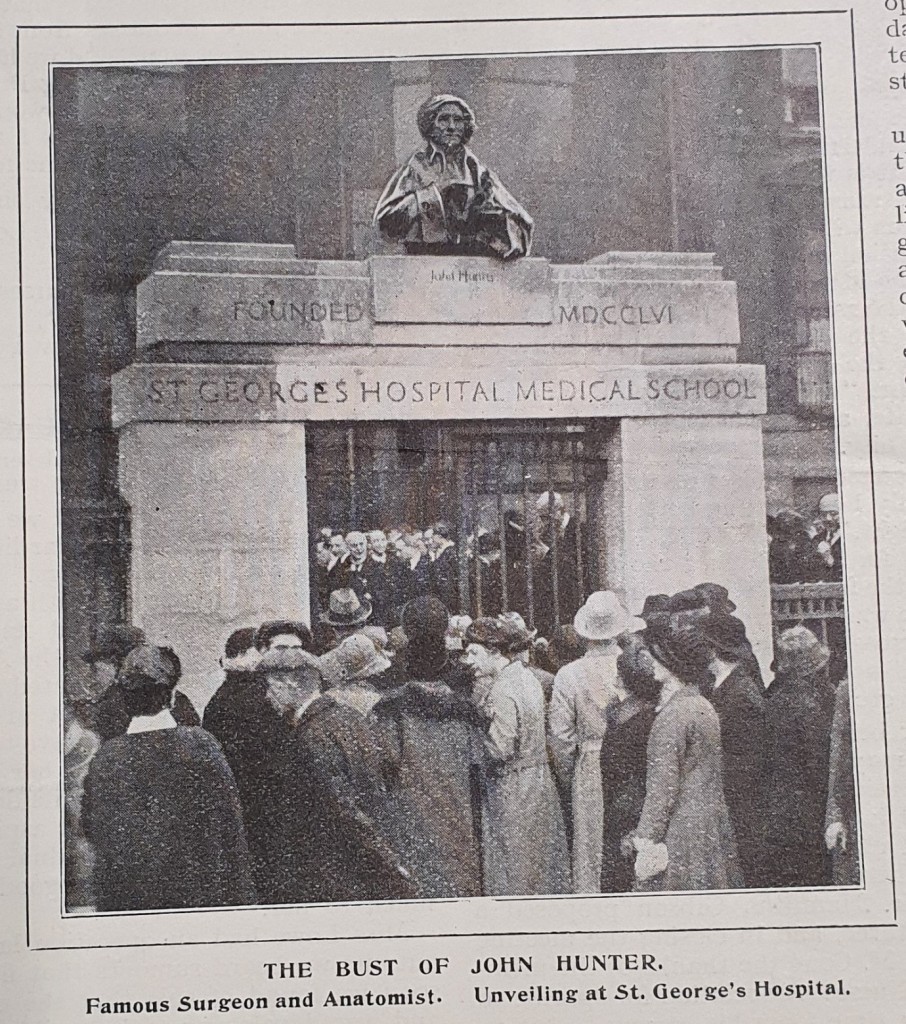
In 1735, St George's Hospital purchased the freehold of Lanesborough House, two adjoining houses and two acres of land. Under the direction of Isaac Ware of the Board of Works, the hospital was enlarged to accommodate 200 patients. By 1825 the hospital was falling into disrepair. A competition was held for the design of a new hospital. It was won by William Wilkins, and the new building was opened at Hyde Park Corner in 1829. Since its foundation, St George's Hospital has been training medical students. In 1834, a medical school was established in Kinnerton Street and it was incorporated into the main hospital building in 1868.
Just before the beginning of the Second World War, it was decided that St George's needed to be rebuilt on its Hyde Park Corner site. The plan was however abandoned by the commencement of hostilities. During the War, against a background of the population shift from central London, discussions took place which paved the way for St George's to be rebuilt and transferred out of the city centre.
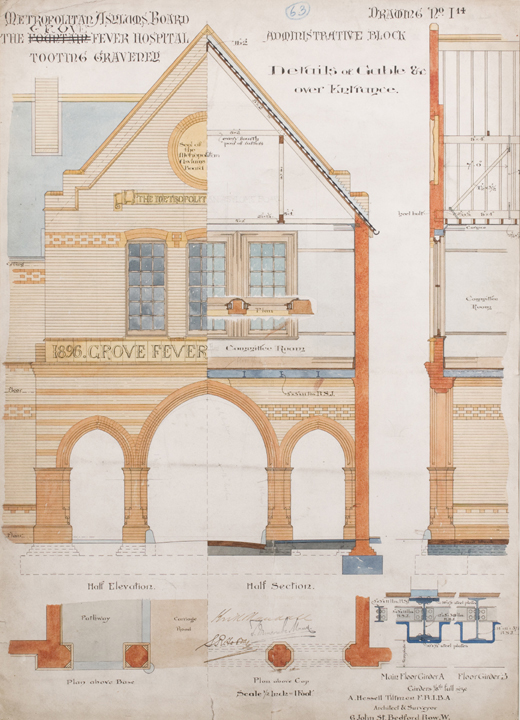
With the introduction of the National Health Service in 1948, the hospital became part of the St George's Hospital Teaching Group of the South West Metropolitan Regional Hospital Board. Soon after, the Board of Governors persuaded Aneurin Bevan, the Minister of Health, that the new hospital should be built on the Grove Fever Hospital and Fountain Hospital sites in Tooting.
Patients began to be admitted into the Grove Hospital in 1951 and, by 1953, the Grove Hospital was designated to St George's and responsibility for it was transferred from the Wandsworth Hospital Group to the Board of Governors of St George's. The Fountain Children's Hospital site adjacent to the Grove Hospital was added to the land available for the St George's Hospital redevelopment when the Fountain transferred to Queen Mary's Hospital, Carshalton.
The building of the new St George's at Tooting, South West London, began in 1973. Following the reorganisation of the National Health Service in 1974, the Board of Governors was disbanded, and the responsibility for St George's Hospital was passed to the Wandsworth and Merton District of the Merton, Sutton and Wandsworth Area Health Authority. South West Thames Regional Health Authority assumed responsibility for the rebuilding of the new St George's. The first phase of the new St George's Hospital Medical School opened in 1976. The hospital at Hyde Park closed its doors for the final time in 1980 and HM Queen Elizabeth II formally opened the new St George's Hospital and Medical School at Tooting on 6 November 1980. Lanesborough Wing, the first of the ward blocks opened in 1980. In 1993, St George's Hospital came under the control of St George's Healthcare NHS Trust.
The hospital has been administered by the following:
- 1733 - 1948: St George's Hospital
- 1948 - 1974: St George's Hospital Teaching Group of South West Metropolitan Regional Hospital Board
- 1974 - 1982: Merton, Sutton and Wandsworth Area Health Authority of South West Thames Regional Hospital Board
- 1982 - 1993: Wandsworth District Health Authority of South West Thames Regional Hospital Board
- 1993 - : St George's Healthcare NHS Trust
From the eighteenth century until the creation of the NHS, medical care for acute and chronic conditions in Great Britain was split between:
- royal or endowed hospitals such as Guy’s Hospital, St Thomas’s Hospital and St Bartholomew’s Hospital that were originally monastic hospitals and were later given a royal charter. These survived on the income from their large investments
- voluntary hospitals, independent hospitals that relied on private funding and philanthropy and which were either general or specialised
- cottage hospitals, which started opening from the 1860s and in which patients were treated for a weekly sum
- asylums
- poor law workhouses and infirmaries, which were run by the government
- dispensaries, which were supported by charities and sometimes required patients to pay for medicine supplied or pay weekly subscriptions
- patient’s own homes where they were visited by private physicians
- The Royal Free Hospital, which did not require a governor’s letter or any form of payment for admission.
From its creation in 1733 until the establishment of the NHS, St George’s Hospital was a voluntary hospital, and as such it was reliant on receiving donations from ‘subscribers’. Lindsay Granshaw explains the way most voluntary hospitals were creating saying:
‘A leading lay figure or group would decide on the need for a hospital; the support of a few aristocrats would then be enlisted, and their names published prominently to encourage those of lower social standing to make donations as well. Friends, relatives and other contacts were also tapped for their support. Donors were given certain benefits. According to the sum contributed, they had the right to admit patients. […] A more sizeable donation would bring multiple rights. In addition, benefactors became hospital governors: they elected a dozen or so of their number to supervise the hospital and they voted for members of staff’.
St George’s Hospital was run by a board of governors made up of those who made large financial contributions to the hospital and medical staff who, unlike at most voluntary hospitals, were eligible to make subscriptions to the hospital. In 1840 this included four physicians, one assistant-physician, four surgeons, two assistant-surgeons, four visiting apothecaries, three teachers from Sir Benjamin Brodie’s Anatomical School and the lecturer on midwifery (The Lancet, 33:857 (1 Feb 1840)). In order to support themselves, voluntary hospitals ‘ran continuous appeals and publicity campaigns’ (Rivett), and voluntary hospitals competed with each other for funding. They would organise dinners and fundraisers which played an important part in the social calendar for donors (Rivett). The expanding middle class would donate to the hospitals out of philanthropy and because of the social status it brought them (Granshaw). After 1897 voluntary hospitals like St George’s Hospital also received funding from the Kind Edward’s Hospital Fund.
Voluntary hospitals were founded on what Geoffrey Rivett refers to as ‘a wave of philanthropy’ in the eighteenth century ‘by those who wished not merely to alleviate distress but to restore the afflicted to respectable and independent citizenhood’. They were intended to treat the ‘sick poor’, or those who could not afford to be treated by private physicians. A distinction was made between the ‘poor’ who were considered to be self-reliant and therefore believed to be deserving of charity and the ‘destitute’ who were not. As Henry Burdett, the hospital administrator who helped to establish the British Hospitals Association in 1884, stated:
‘The object of the hospitals is to cure with the smallest number of beds the greatest number of cases in the quickest possible time. The people who are entitled to free relief are those who are able to maintain themselves independently of all extraneous assistant until the hour of sickness, when the breadwinner, for instance, is struck down, or the added expense of sickness in the home renders it necessary that the hospital of dispensary should step in’ (Rivett).
As Anne Borsay explains, the voluntary hospital ‘shared with the workhouse a commitment to economic rationality. Instead of putting the poor to work, hospitals sought to render them healthy for useful employment, thereby increasing national prosperity and reducing the cost of relief’.
As such, a patient’s eligibility for admission to St George’s Hospital was judged based on both medical and ‘social economic considerations’ (King Edward’s). To be treated as an outpatient or an inpatient at a voluntary hospital, patients needed a letter from one of the hospital governors or a hospital subscriber that said that they were ‘proper objects of charity’, although this rule gradually became less enforced and by 1910 St George’s Hospital reported that it was not required for outpatients (Louden)). The only exception to this was the Royal Free Hospital, which started as a dispensary and from 1833 became a voluntary hospital established specifically to treat patients for free without a subscriber’s letter.
While St George’s Hospital was located at this time in a wealthy part of London, at Hyde Park corner, the majority of its patients were from the working classes. They mostly came from Westminster and Pimlico, both of which were largely poor, working class areas and some parts of which were slums. In 1910 St George’s Hospital reported that the majority of outpatients came from Westminster (Pimlico), Chelsea, Fulham and Battersea, with a few coming from further South in Clapham, and Lavender Hill (King Edward).
The 1834 new Poor Law removed outdoor poor relief and outlined four types of pauper, ‘the aged and really impotent’, children, ‘able-bodied females’ and ‘able-bodied men’ and ‘proposed distinct institutions’ to deal with each of these groups. It did not, however, define the term ‘impotent’, nor did it ‘suggest any alternative to the existing practice of providing the sick poor with relief in their homes’. The result was that people with disabilities, people with chronic or acute illnesses, and the elderly were forced to seek accommodation and care in workhouses if they or their families could not support them by working (Workhouses.org.uk). These people could, however, be treated in voluntary hospitals when an accident had taken place or surgery was required, as Poor Law Commissioners wanted to discourage operations taking place within workhouses. In 1866, ‘a total of 21,000 sick and aged inmates’ were being treated in workhouses. Workhouse infirmaries were built to accommodate these people, and people with mental disabilities were transferred to asylums (Workhouses.org.uk). Medical care in these infirmaries was so poor and so heavily criticised that in 1867 the Metropolitan Asylums Board was created to try to improve health care provision for the sick poor.
In the last third of the nineteenth century, as the ‘destitute’ became increasingly treated in workhouse infirmaries built by the Metropolitan Asylums Board, voluntary hospitals like St George’s also became more popular with the lower-middle-classes (Granshaw). Despite the fact that reports showed that in the 1860s it was safer to be treated in a hospital in London than in Paris (Rivett), hospitals were, however, associated with infection, dirt and a lack of ventilation and so those who could easily afford to pay for a private physician chose to be treated at home, and the medical system was designed so that people who could afford to be treated outside of a hospital should be. When cases of upper-class patients are found in the post mortem casebooks for St George’s Hospital it is usually because they were injured in an accident nearby or were brought in dead.
This selection of patients for voluntary hospitals to treat was, however, not only the result of social ideologies. It was also necessitated by material considerations. Demand for treatment far outweighed the number of beds and amount of funding available, especially as the population of London grew. Whereas in the early eighteenth century when St George’s Hospital was founded the population of London was half a million, by 1800 it was one and a half million, and by 1900 it had risen to five million (Granshaw). Hospitals also had to prove their efficacy in order to appeal to donors and receive funding.
As a result, voluntary hospitals became increasingly selective about the type of illnesses they would treat, ‘choosing those who would benefit rapidly, particularly from surgical treatment’ (Rivett). Focus was placed on the curable. In evidence given to King Edward’s Hospital Fund for London in 1910, a representative for the St George’s Hospital justifies this by saying that ‘The aim is to restore the patients to health and fit them once more to earn their living. It follows that those in receipt of Poor Law relief and others who are suffering from chronic and incurable maladies are not fit and proper objects of the Charity, and where this fact is known and no harm would result, the patient is refused treatment and referred to the Poor Law. Where the case is more urgent, but still incurable, they are treated first and dealt with in the same way’. He went on to say, however, that when a patient was considered to suffer from something incurable but that could be relieved they would be treated for some time. Patients who visited St George’s and then needed time to convalesce and who were considered ‘proper objects of charity’ were then sent to Atkinson Morley Convalescent Hospital, which was created by St George’s using a legacy from Atkinson Morley, a former student, or to other convalescent homes that the almoner could refer them to who were willing to take convalescent patients at a reduced cost (King’s).
As well as taking into account medical and social economic considerations when deciding on who was suitable for treatment, admissions might also be affected by moral and religious attitudes. People who were considered to be responsible for their condition, such as ‘fallen women’ with venereal diseases, might be refused treatment at voluntary hospitals. Since the mid eighteenth century the Lock Hospital had existed to treat venereal diseases and there had also been the Magdalen Hospital for Penitent Prostitutes.
The result of this system was ‘inequality of access to health care’ with ‘resources being skewed towards younger adults and men among whom short-term ailments were most prevalent and economic utility most pressing’ (Borsay). Many people found themselves excluded from health care, including ‘socially “undeserving” patients’, […] children, pregnant women, fever cases, lunatics and incurables’ (Granshaw).
An increasing number of specialised voluntary hospitals and dispensaries were built by doctors specifically to treat these groups, and ‘[b]y the 1860s there were at least sixty-six special institutions in London alone’ (Granshaw). These included lying-in hospitals for married mothers, children’s hospitals, orthopaedic hospitals, eye hospitals, fever hospitals, and hospitals to treat patients with tuberculosis or cancer. As these specialised hospitals began to pose more competition for funding in the mid nineteenth century general voluntary hospitals like St George’s began to create eye departments, ear departments, and orthopaedic departments (Granshaw).
General voluntary hospitals were reluctant to treat fever cases because they might lead to outbreaks within the hospital and, as a representative from St George’s testified to the King Edwards’ Fund for Hospitals in 1910, they did not have ‘the space to admit and isolate these cases’. From the beginning of the nineteenth century specialised voluntary fever and smallpox hospitals were established, and from the 1890s the Metropolitan Asylums Board started building more (as well as large asylums). These included two hospitals that used to stand on the grounds that the current St George’s campus is on in Tooting: the Fountain Hospital (which was built after an outbreak of scarlet fever in 1892 and 1893 and later became a mental hospital) and Grove Fever Hospital (which was finished in 1899). Nevertheless, patients with measles, whooping cough, mumps, chicken-pox, and tuberculosis were often treated as outpatients at voluntary hospitals, a fact which the representative from St George’s in 1910 argued that he believed led to the spread of such diseases.
In the post mortems we do see some cases of these infectious diseases in people who were inpatients but apart from perhaps the amount of patients suffering from tuberculosis, the numbers do not reflect the prevalence of these conditions at the time. We also do not tend to see case numbers rise particularly in the years that there were epidemics. The exception to this is the volume for 1854 – the year of the Broad Street cholera epidemic – in which there are two pages of the names of patients who died from cholera but for whom post mortems could not be carried out due to the high number of deaths.
When patients with smallpox were admitted to St George’s it seems to have been because the disease was not immediately identified. When it was they were moved to separate wards with their bed and bedding and then moved to a smallpox hospital to prevent outbreaks. When there were outbreaks of infectious diseases at the hospital these seem to have been reported in the Lancet. One such outbreak of smallpox at St George’s was reported in the Lancet in 1871, with the writer noting that the hospital construction was ‘extremely faulty’ for preventing the spread of infection as ‘The staircases and corridors are huge reservoirs of air, which, if infected, from any cause whatever, is diffused to every ward’ as in the staircases there ‘is a strong upward draught, by which air is drawn up from the basement, and the surgical wards and other rooms on the ground floor, and, after being mixed with that in the corridors, passes into all the wards above’. The arrangement of the hospital, they wrote, did ‘not compare advantageously with a modern workhouse hospital’ (The Lancet, 97:2475 (1871)).
The Public Health (London) Act of 1891 made it a requirement for public health authorities to be notified of cases of smallpox, cholera, typhoid, diphtheria, membranous croup, erysipelas, and scarlet fever. Tuberculosis was not included on this list despite the fact that in 1882 the bacteria responsible for causing the disease had been discovered by Robert Koch. This was the result of lingering beliefs about the role heredity and constitution played in acquiring the disease which seemed to be the only way to explain why only some people who were exposed to the disease became sick (Cantor).
As a general voluntary hospital you see a wide variety of types of ailment being treated in the patient records from St George’s Hospital. As a result of voluntary hospitals’ focus on the curable, however, the majority of cases treated were for acute rather than chronic conditions. In 1822 Sir Gilbert Blane listed ‘intermittent fevers, rheumatism, dropsy and continued fever’, as well as ‘chronic tuberculosis’, ‘tumours at an advanced stage, bladder calculi and the late results of syphilis’ as being the most common conditions seen in voluntary hospitals, and this is reflected in the causes of deaths of patients in the St George’s post mortem casebooks (Rivett).
In the early nineteenth century, surgery formed only a very small amount of the work done by hospitals. At St George’s Hospital surgeries were conducted one day a week, which in 1854 was on Thursdays. The discovery of general anaesthesia and efforts to bring down the mortality rate from sepsis, however, led surgeries to become more common. Attempts to prevent post-operative infections were inhibited by the fact that germ theory ‘was far from accepted’, but ‘by the twentieth century the amount of surgery was increasing very rapidly and came largely to dominate the business of hospitals’ (Granshaw).
The post mortem casebooks contain many cases of patients who died following occupational accidents, many of which were railway accidents. Patients who were injured as a result of work at the shipyards and warehouses at the docks would have been sent to London Hospital.
While the post mortems do contain cases of patients with chronic illnesses and physical and mental disabilities, generally they have been admitted because of the onset of an acute condition or because their symptoms have suddenly become more severe. As the eighteenth and nineteenth centuries progressed the number of hospitals, asylums, and, after the introduction of compulsory schooling in 1880, schools that were built to house people with disabilities multiplied, and particularly throughout the nineteenth century people with disabilities were increasingly institutionalised.
St George’s published its figures in the Lancet and the archive also holds the hospital’s annual reports.
Salaries at hospitals like St George’s were not well paid, and fees paid by students made up a large part of physicians’ and surgeons’ wages. At St George’s Medical School, surgeons would receive 700l per year and physicians 400l per year from students. Two physicians and two surgeons would also give lectures for which they would receive large fees (The Lancet). Hospital doctors would frequently also have private practices to supplement their income, and they used their roles in respectable hospitals to build their reputations and so ‘hospital positions which afforded such teaching possibilities became ever more sought after’ (Granshaw). Some hospital staff would also work in specialist hospitals alongside holding positions at general hospitals like St George’s.
Doctors would publish interesting cases they had treated in medical journals such as the Lancet, the British Medical Journal, Transactions for the Pathological Society of London, and the Edinburgh Medical Journal. The Lancet contained a section entitled ‘A Mirror of the Practice of Medicine and Surgery in the Hospitals of London’ which would contain descriptions of patients treated at St George’s Hospital. Frequently cases from the post mortems were featured in these journals, and sometimes the post mortem includes a printed copy of the article or has an annotation stating where it can be found.
In the early nineteenth century, matrons ‘were usually respectable widows’, but the rest of the nurses ‘were generally recruited from the poorer classes, frequently from among the patients themselves’. As Granshaw notes, there were ‘strong parallels’ between nursing and domestic service at the time, with ‘cleanliness and discipline’ being considered paramount for both roles. It was not an easy job, nurses ‘undertook menial tasks, their turnover was high, they were paid on a weekly basis, and they were sacked without notice’. By the end of the nineteenth century it has been argued that nurses tended to be from middle-classes, however, a study of nurses at St George’s Hospital by Sue Hawkins has shown that while this was the case for a larger percentage of nurses, ‘nearly 40% of St George’s nurses could be described as having a working class background’. This was even the case for matrons, suggesting that at least at St George’s ‘a career in nursing could lead to promotion and advancement for women from less advantageous backgrounds’.
While nursing care in early nineteenth century is frequently criticised, nursing in London voluntary hospitals had the reputation at the time of ‘providing “the best that the knowledge and the practice of the times permitted”’ (Rivett). Its bad reputation stems perhaps from the efforts of nursing reformers like Florence Nightingale ‘in the second half of the nineteenth century’ who ‘vehemently stressed the darker side of earlier nursing in order to emphasize the case for reform’ by ‘point[ing] to real and imagined cases of drunkenness, dishonesty, immorality, corruption and laziness among nurses, suggesting that all were like that’ (Granshaw). With nursing reforms and the increasing literacy of nurses after elementary education became compulsory in 1876 the image of nurses improved, and by the end of the nineteenth century they were pictured as ‘clean, neat, disciplined, uniformed’ and ‘trained in nursing schools’, which helped to make hospitals more attractive to the middle classes (Granshaw).
By Alexandra Foulds. This text was originally published as 'Outpatients at St George's Hospital, 1733-1948', St George's Library blog, 29 Apr 2021.
How did you become an outpatient at St George’s Hospital before the creation of the NHS? What was it like to be an outpatient at St George’s Hospital at this time? Well, from its establishment in 1733 until the creation of the NHS in 1948, St George’s Hospital was what was called a voluntary hospital, which meant that it was reliant on receiving donations from ‘subscribers’ for funding. The board of governors at St George’s Hospital was made up of those who made large financial contributions to the hospital and medical staff who, unlike at most voluntary hospitals, were eligible to make subscriptions to the hospital.
In order to support themselves, voluntary hospitals ‘ran continuous appeals and publicity campaigns’, and voluntary hospitals competed with each other for funding. They would organise dinners and fundraisers which played an important part in the social calendar for donors. The expanding middle class would donate to the hospitals out of philanthropy and because of the social status it brought them. Becoming a subscriber to a voluntary hospital also meant that you could refer people to the hospital to become an outpatient or inpatient, and the amount donated equated to a certain number of referrals that were allowed per year.
Voluntary hospitals were created in the eighteenth century to give free medical treatment to the ‘sick poor’, or those who could not afford to be treated by private physicians. A distinction was made between the ‘poor’ who were considered to be self-reliant and therefore believed to be deserving of charity and the ‘destitute’ who were not. As Henry Burdett, the hospital administrator who helped to establish the British Hospitals Association in 1884, stated:
‘The people who are entitled to free relief are those who are able to maintain themselves independently of all extraneous assistant until the hour of sickness, when the breadwinner, for instance, is struck down, or the added expense of sickness in the home renders it necessary that the hospital of dispensary should step in’.
This meant that initially to be treated as an outpatient or an inpatient at a voluntary hospital like St George’s, patients needed a letter from one of the hospital governors or a hospital subscriber that said that they were ‘proper objects of charity’, and even once patients had been accepted they were subject to suspicion that they may be abusing the system.
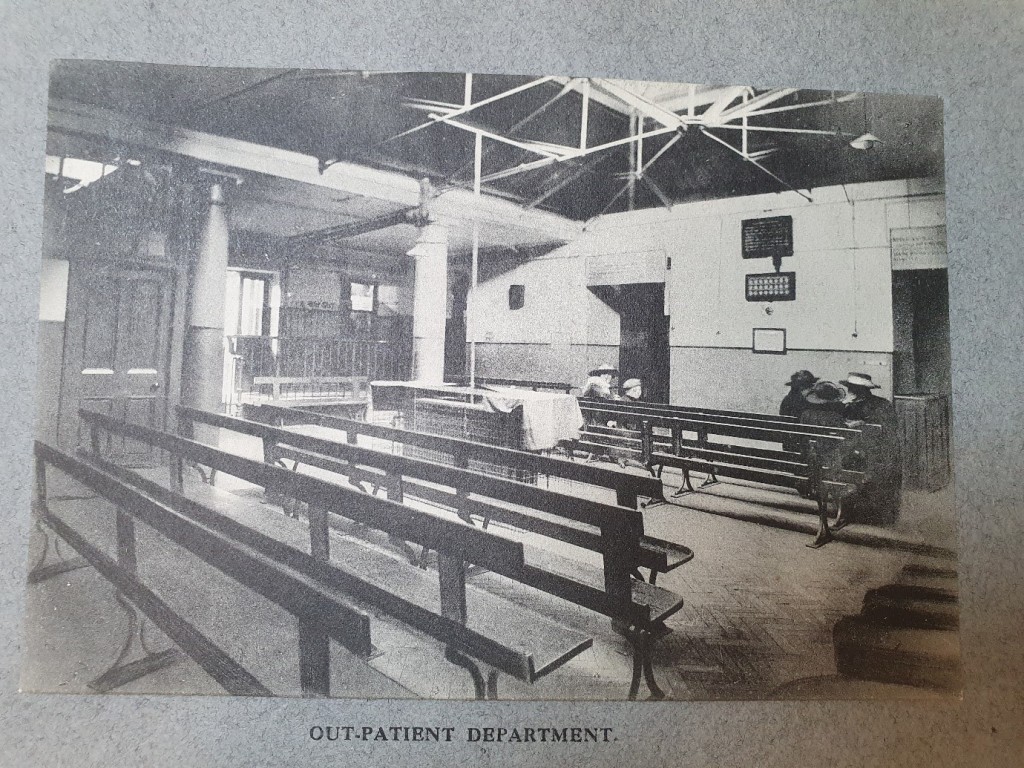
The outpatient department functioned alongside dispensaries to provide out of hospital medical care to poor patients on a charitable basis, and it was where the majority of what we now refer to as primary care was conducted.
Patients at St George’s mostly came from Westminster and Pimlico, both of which were largely poor, working class areas and some parts of which were slums. In 1910 St George’s Hospital reported that the majority of patients came from Westminster (Pimlico), Chelsea, Fulham and Battersea, with a few coming from further South in Clapham, and Lavender Hill (King Edward). 6% of these patients were trained servants, however, only 2 1/4% were currently employed as servants, and their average annual wage was between £21 and £22.
After receiving a letter from a subscriber to the hospital, outpatients would visit St George’s Hospital. They would first be seen by a Medical Officer who would decide whether a patient was an acceptable hospital case, should be an outpatient or an inpatient, or should be treated as a casualty in which case they would be seen by a doctor immediately. The term casualty could apply to anything from ‘a small cut’ to a ‘bad toothache’, as well as those who had been in an accident. Once a patient had been accepted as an outpatient an Inquiry Officer would ask for their name, age, occupation, address, their marital status, their wages, and if they were married then their number of children that were dependent on them. In the case of patients who were children they would also be asked for information about the father, and in the case of married women they would be asked for information about their husbands.
Upon their second attendance at the hospital they would be seen by a Casualty Officer and an Almoner. The almoner could then investigate to advise on whether free treatment should be ceased and patients should be referred to workhouse infirmaries, private practitioners, dispensaries, or other hospitals. In 1910, of the 48,583 outpatients 6,768 cases were investigated, with 432 considered not suitable for treatment. The almoner could also decide along with the doctor whether home visits from volunteer ‘lady health visitors’ should be organised, or whether instruments (such as trusses for hernias) or meals should be provided, generally paid for out of the Hospital’s Samaritan Fund which was principally made up of subscriptions from hospital governors. The almoner was also responsible for coordinating with charitable societies to ensure that patients would continue to receive the care they needed outside of the hospital.
At the beginning of the nineteenth century, outpatient treatment numbers were small, however, from 1835 they began to rise and continued to rise until the beginning of the twentieth century. In the years 1833-1842, St George’s Hospital treated 70,000 cases of which 44,000 were outpatients. By 1910, St George’s treated 48,583 outpatients in that year alone, of which 67% were casualties.
As a result, doctors had to treat patients incredibly quickly, with Dr Robert Bridges, a casualty physician at St Bartholomew’s Hospital and later the Poet Laureate, writing in 1878 that he had to treat over 30,000 outpatients a year at a rate of 88 seconds per patient. By 1900, St George’s Hospital introduced a limit on how many new outpatients would be treated each day with the rest being turned away. In 1910 average outpatient attendances were approximately 160 a day, with new cases limited to 15 per hospital department per day, with all patients being seen first by a superintendent who imposed the limit when they arrived at the hospital. If a patient was not one of the 15 but was considered to require treatment he was brought back the next day.
As outpatient departments provided free access to health care, they were viewed as being in competition with private physicians and were therefore seen as a threat to the physician’s income. This meant that in medical journals outpatient departments, and voluntary hospitals more generally, were frequently described as locations in which patients abused the medical system by getting free care when they could afford to be treated by a private doctor.
By the end of the nineteenth century several voluntary hospitals, St George’s among them, was choosing not to require a letter from a hospital subscriber for outpatients (Louden), and so physicians tried to introduce the requirement for patients to be referred to the hospital by private practitioners in order to prevent this perceived abuse of the system. A letter to the British Medical Journal in 1894 stated that:
‘The abuse of the hospitals’ outpatient departments is an evil so gigantic that the tendency is to regard it […] as necessary in the sense of being unavoidable […] The remedy lies in the hands of those who suffer most from the unfair competition of the hospitals, and it is idle to appeal to the public or to the hospital authorities. […] The remedy I would suggest (though I claim no originality) would be to admit to the outpatient department only patients whose cases are certified by some medical authority or medical man to require special consideration’.
In 1910, however, only 3-6% of outpatients at St George’s Hospital were referred by physicians.
These perceived abuses led in 1910 to an investigation into the admission of outpatients in hospitals in London by the King Edward’s Hospital Fund for London, who from 1897 gave funding to voluntary hospitals. They called on people from various medical charities and representatives from each of the voluntary hospitals to testify, asking about the suitability of the letter system, hospital procedures for dealing with outpatients, the numbers of outpatients and the kinds of cases hospitals treated, and whether they believed the system was being abused by patients. William West, the treasurer at St George’s at the time, testified, arguing that he did not believe that the system was abused at St George’s, but that there were times it was misused by patients who had paid to be treated by a physician and upon seeing no improvement wanted a second opinion and so visited the hospital.
In 1948 the NHS Acts brought voluntary hospitals under public ownership, however, researchers have argued that it is these nineteenth and early twentieth century arguments about the relationship between hospitals and private physicians that led to our current NHS health system in which patients are required to be referred to specialists in hospitals by their GP.
Voluntary hospitals like St George’s Hospital were also important sites for medical education and scientific research and were viewed as being at the cutting edge of medicine. They were the place where experimental treatments could be tested as the patients were ‘[p]oor and unable to complain’, and ‘lessons learned from them could be applied to better-off patients’ (Granshaw).
The nineteenth century has been described since the criticism of Michel Foucault as being a time in which medical education shifted and moved out of the lecture theatre and into the hospital. At this time, humouralism or the belief that illness came from an individual imbalance of vital bodily fluids became replaced by pathology and the idea that all illness could be traced to lesions found through post mortem examinations. As a result, post mortems became a fundamental part of hospital medicine and medical education with the understanding that ‘[a]fter identifying pathological conditions in cadavers through physical change in the organs, the same condition was to be recognized in the living, if possible through signs which were independent of symptoms’. With the discovery of cells and later of germs, this then became ‘replaced by laboratory medicine’ from 1848 as microscopical analysis and bacteriological testing became eminent (Granshaw). These shifts in the understanding of ill health meant that the focus of doctors ‘shifted from the whole body to the diseased part’, with emphasis placed ‘less on symptoms reported by the patient, now seen as subjective, and more on signs that could (in theory) be objectively measured, often with the use of instruments’.
Experience working in a hospital became a requirement in order to be a licensed medical professional. To become a licensed by the Royal College of Surgeons, ‘a year’s experience in walking the wards was required’, and ‘[i]n 1815 the Apothecaries’ Act laid down that anyone applying for the licentiate of the Society of Apothecaries must walk the wards for six months’. The 1858 Medical Act also helped to put hospitals at the centre of medical education (Granshaw).
Blomfield, Joseph. 1933. St George’s 1733-1933. Medici Society.
Crellin, John K. 1961. “Eighteenth Century Pharmacy at St George’s Hospital, London”. Medical History 5(4): 327-340.
--- 1962. “Apothecaries, Dispensers, Students and Nineteenth-Century Pharmacy at St George’s Hospital, London”. Medical History 6(2): 131-145.
Dent, Clinton. 1894. “History of Nursing at St George’s Hospital.” St George’s Gazette 13 / 14 / 15 (II): 41-49 / 61-70 / 82-88.
Gould, Terry, and David Uttley. 2000 (1997). A Short History of St George’s Hospital and the Origins of Its Ward Names. Continuum International Publishing Group Ltd.
Gould, Terry, and David Uttley. 2000. A History of the Atkinson Morley’s Hospital 1869-1995. A&C Black.
Hawkins, Susan. 2007. “Myth and Reality: Uncovering and Discovering the Nurses of St George’s Hospital, London 1850-1900.” Kingston University.
--- 2010. ‘From Maid to Matron: Nursing as a Route to Social Advancement in Nineteenth-Century England’, Women’s History Review, 19(1): 125-143.
Higginbotham, Peter. ‘The Fountain Hospital, Tooting’. The Workhouse: The story of an institution… http://www.workhouses.org.uk
--- ‘The Grove Hospital, Tooting Grove’.
Hunter, M.I.A., T.R. Gould, and R.F. Fairweather. 1983. St George’s Hospital and Medical School and Associated Hospitals 1933-1983.
James, R.R. 1928. The School of Anatomy and Medicine Adjoining St George’s Hospital 1830-1863.
Page, William Emanuel. 1866. St George’s Hospital... : Some Account of the Hospital and School.
Peachey, George C. 1910-1914. The History of St George’s Hospital. London: J. Bale.
Sisley, Richard. 1893. “History of Nursing at St George’s Hospital”. St George’s Hospital and Medical School Gazette 2 (13): 41–49.