Cases from the post mortems
View all Close all
By Alexandra Foulds. This text was originally published as 'The Case of the Monkey on the Railway', in Railway Work, Life & Death, 15 Mar 2021.
At the end of 2017 St George’s University of London received funding from Wellcome to conserve, digitise and catalogue the archive’s collections of post mortem examinations and casebooks. These were created by St George’s Hospital and Medical School between 1841 and 1946 and they contain the medical case notes and post mortem reports from patients that died at St George’s Hospital in this period, which at the time was located at Hyde Park Corner.
St George’s Hospital was a voluntary hospital, which meant that the majority of its patients were from the lower classes as wealthier patients could afford to be treated by visiting doctors in their homes. The casebooks list the occupations of the patients, and a great deal of them worked for the railway as brakesmen, guards, foremen, clerks, inspectors, shunters, signalmen, signal-fitters, engine cleaners, engine fitters, and engine drivers. Many of these died from internal causes or as a result of diseases that were endemic in the period, such as tuberculosis, but there are also a lot of cases of patients dying as a result of occupational accidents. St George’s Hospital proximity to Victoria Station also meant that any injured passengers were often transferred to the hospital.
Image of PM/1897/269 (John Harris), St George’s University of London Archives, Creative Commons CC-BY License
As a result, the railway is frequently mentioned in the post mortem casebooks, however, when cataloguing the 1897 volume one of our project archivists came across a railway-related monkey mystery that left us baffled. In the case notes for 31-year-old John Harris, admitted to St George’s Hospital on Friday the 3rd of September 1897, had been written:
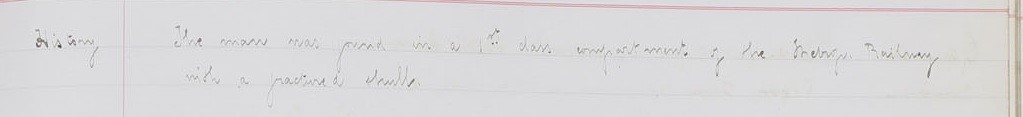
‘This patient was climbing on to a railway (after a monkey) and was thrown with great violence on to the platform. There is an extensive fracture of the skull, comminuted and partly depressed behind the left parietal eminence. Laceration and protrusion of the brain. Mr Sheild removed pieces of bone and elevated others. The patient did not rally and died shortly after’.
The cause of Harris’s death is given as ‘fractured skull, lacerated brain’, and the post mortem exam shows that all of his extremities were intact, but Harris had a hole ‘3 ½ inches in length and 1 ½ at the widest and lowermost points’ in his skull and other skull fractures. It also tells us a bit about what Harris looks like, with the examiner noting that he was ‘a well built muscular man […] Height 5ft 4 ½ inches’ with a ‘short red beard – red moustache and hair’.
The patient’s occupation is not listed, however, and there is no explanation at all in the casebook about why he had been chasing a monkey or how exactly he was ‘thrown’ on to the platform.
The Twitter conversation that started this blog post!
When we posted about the case on social media it left certain railway enthusiasts *cough* demanding more. While unfortunately (or maybe fortunately?) this seems to be the only monkey-railway-accident in our collection, we can reveal the results of our detective work into who John Harris was and what happened to him, and why a monkey was on a train. We had to know: was there a great monkey zoo escape in London in 1897 and Harris was a zookeeper? Was this a case of monkey murder? Was there an attempted Planet of the Apes uprising in 1897?
There was an inquest into Harris’ death on Monday the 6th of September 1897 held by the Westminster coroner, which was reported on Saturday the 11th of September in the Yarmouth Independent in a section forebodingly called ‘Train Dangers’. The article reveals that Harris was ‘a petty officer of the cruiser Racoon’ who had been travelling on a special ‘with a number of other sailors from Sheerness to Victoria’ when ‘he suddenly clambered out of the window, and the next seen of him was when he was hurled, apparently from the roof of the carriage on to the line as the train ran through Clapham-road Station’. The only witness to speak at the inquest was a porter at the station who said that he had ‘had his back to the train’ when ‘he felt some pieces of wood strike him on the back of the head, and on turning sharply round he saw the deceased came down on his feet, but was unable to keep his feet, and staggered back against the train’. Harris was then struck on the head multiple times by the footboard of the train until he was eventually thrown on to the side of the rails’. When he was found he was unconscious but breathing and he was transported by train to Victoria station and from there to St George’s Hospital.
The newspaper article states that he died on the journey, however, this contradicts the medical notes from the case which shows that Harris arrived at the hospital alive and underwent surgery. The post mortem examiner comments on ‘a triangular wound (surgical) […] from which project two drainage tubes’ and says that elsewhere on the parietal bone ‘in two places the marks of trephine are visible’. Clearly the doctors at St George’s tried to reduce the pressure on Harris’s brain. Also, despite the mention of the monkey in the doctor’s case notes, there is no indication that the monkey was discussed at all at the inquest. It seems that the coroner was not presented with the whole story, and according to the newspaper article the coroner and jury at the inquest gave a verdict of ‘accidental death’ after judging the evidence ‘to be of a very flimsy character’.
A second article from the Globe on the following Thursday the 16th of September, however, finally sheds some light on the role of the monkey in the case and why Harris climbed on to the roof of the train. It says that the coroner had received more information about Harris’ death. Apparently, when Harris’ ship the Racoon had been ‘stationed off the West Coast of Africa, Harris bought a baby monkey. This soon became the pet of the crew, owing to its tricks’. Harris, we are told, ‘brought the monkey home with him, and when he got into the carriage at Sheerness’ on the day in question ‘the monkey was with him’. On the journey ‘All the occupants of the carriage were larking with the monkey, when suddenly, when nearing Clapham-road station, it snatched a scarf from one of the blue-jacket’s necks and bolted out of the window’. When this happened, it is reported that ‘Harris at once said he must try and get his pet back, as otherwise it might be killed’ and ‘Although his companions tried to dissuade him, and told him of the risk he was running, he said he would rather lose his life than his pet’ and so he ‘at once clambered out of the window’, where it is thought that he ‘must have lost his hold’ and fallen. What became of the monkey and whether it survived or was ever retrieved is unclear.
The mystery of the monkey then turns out to be a story of devotion to a pet, set against a backdrop of nineteenth-century imperialism and commercialism. The monkey was vindicated, although it is maybe not quite a case worthy of Sherlock Holmes.
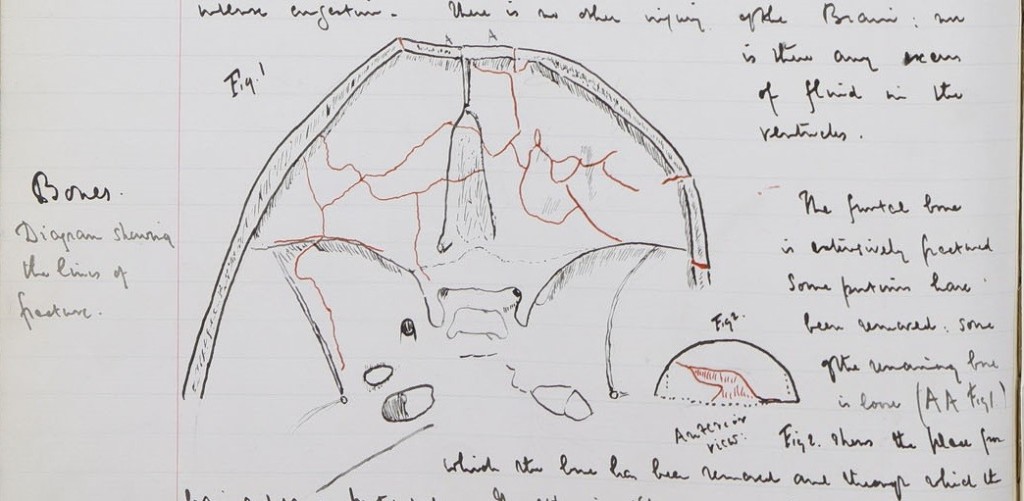
While this is the only monkey-related case in St George’s post mortem collection it is, however, not the only railway enigma. In the volume from 1886 there is the case of 47-year-old Moritz Fischer, who was found ‘with a fractured skull’ in an empty 1st class compartment of a Metropolitan Railway train. A case for Agatha Christie perhaps? This is the next railway-related death that the St George’s Archives detective team will be looking into.
By Natasha Shillingford. This text was originally published as 'A Railway Mystery', St George's Library Blog, 7 Apr 2021.
See full case notes here: PM/1886/292
Following on from the discovery of a post mortem case of a monkey on the railway we decided to explore other cases of railway mysteries in the post mortem collection of St George’s Hospital. We soon came across a case worthy of the great Hercule Poirot.
On 23rd September 1886 Moritz Fischer was admitted to St George’s Hospital with a compound depressed fracture of the skull, with laceration of the dura mater and brain with meningitis.
 PM/1886/292. Archives and Special Collections, St George’s, University of London
PM/1886/292. Archives and Special Collections, St George’s, University of London
The case notes said that ‘The man was found in a 1st class compartment of the Metrop[olitan] Railway with a fractured skull.’ He was conscious but did not speak. There was a scalp wound about eight inches in length which extended from the centre of the forehead. The external table of the skull was fractured and the internal table was driven through the dura mater into the brain, with the brain substance protruding. The fragments of the bone were picked out with forceps and the scalp was brought together with sutures. He went on well without any special symptoms for nine days when he passed his urine into the bed and became drowsy. His temperature slowly rose from 99 degrees to 106 degrees on the evening of the 3rd October and he died on the 4th.
The post mortem examination states that there was a wound 3 ¼ inches long over the frontal region. It started from a point 1 inch to the right of the middle line and passed obliquely forwards and to the left. The angles of the wound were infiltrated. Beneath it, part of the temporal bone was absent. Some soft greyish substance protruded which was examined microscopically and found to consist almost entirely of nerve fibres, blood and granular matter.
 PM/1886/292. Archives and Special Collections, St George’s, University of London
PM/1886/292. Archives and Special Collections, St George’s, University of London
What happened to Mr Fischer in the first-class compartment to cause such brutal and deadly injuries?
Lloyds Weekly London Newspaper reported on September 26th 1886 that on the arrival of the train at Bayswater, ‘the attention of the newspaper boy attached to the bookstall on the platform was attracted to the last compartment by one of the first-class carriage fourth from the engine, there being a stream of blood on the outside of the carriage door, the window of which was open. On looking through into the compartment the lad observed a gentleman lying prostate on the floor, alone, and with his feet towards the door, there being a small quantity of blood on the carpet, and a much larger quantity on the cushion of the seat nearest the engine.’ The acting-inspector on duty opened the door and ‘saw that the unfortunate man was quite insensible, and that blood was flowing from a terrible wound on the forehead.’ The gentleman was ‘attired in a grey overcoat, the coat underneath being of black diagonal cloth, and his trousers were light-striped. His gold watch and chain were safe, as were also his rings, but not much money was found in his possession. A few papers were discovered, and they were all in German. A visiting card was found bearing the inscription, “Mr. Moritz Fischer,” and the police, as the result of subsequent inquiries, ascertained on Friday that the injured gentleman was Mr. Moritz Fischer, head of the firm of Mr. A. Fischer and Co., general foreign agents of 35 Carter-lane, and having residence in Westbourne-terrace.’ Thus it appears that none of Mr Fischer’s belongings were stolen so theft was unlikely to be a motive for an attack. However, ‘It was reported that despite the carriage being empty, they could not be quite certain on the point, owing to the confusion which prevailed.’ Therefore it is entirely possible that another individual was in the carriage with Mr Fischer and escaped during the turmoil.
The police, however, were of the opinion that Mr Fischer sustained his injuries by accident, and the following anecdote appeared to confirm this hypothesis:
‘A friend of the injured man says that about twelve months ago Mr. Fischer met with a curiously similar but by no means so serious an accident while travelling on the railway. He had put his head out of the carriage window when he was struck by some projection in the tunnel. He was severely cut, and had to wear a bandage for some time. The injury then sustained was just over the forehead, as now, but the skull was not fractured. The old accident subsequently formed a standing joke among his friends, and he was often rallied about putting his head out of carriage window and advised not to be of so inquisitive a turn of mind. Only a few nights ago the old joke was repeated to him, along with the question whether he had lately been putting his head out of the window. This may be an explanation of the mystery, or it may be only a striking coincidence; but it is a singular fact that most of the known facts appear to lend themselves to such an explanation of what at first appeared to be a very tragic crime.’
The newspaper paper continues by saying that ‘It is conjectured that Mr. Fischer had a propensity for watching the people who occupied the adjoining compartments, and while indulging in this habit he must have placed his feet on the carriage seat, and in his endeavour to place his body as far outside the window as possible, his head must have come in contact with the projection in the spring of the arch.’
However, at the inquest into the death of Moritz Fischer (reported in the London Evening Standard 08 October 1886), a friend of the deceased, Fritz Mercier, said that despite being aware of Mr Fischer previously having injured his head during a journey from Manchester, he refuted the claim that he was well known to have put his head out a carriage window. Despite this, the inquest further confirmed that there was no sign of a struggle, there was no derangement of the carriage and ‘On the night of the accident when the traffic had ceased, Witness went in a carriage and found at the very spot where it was supposed the gentleman met with his injury, that it was quite possible by leaning about 18 to 20 inches out of the window, to meet with a similar accident. At the same spot there was a continuous trail of blood on the wall.’ Furthermore, a witness spoke to picking up a pair of spectacles about twenty yards from where the blood was found on the wall, and another witness testified that Mr Fischer had never been known to be without his spectacles.
Based on the evidence, and despite conflicting testimonies from the friends of Mr Fischer, the jury returned a verdict of Accidental Death. Foul play or a case of curiosity killed the cat, either way please refrain from putting your head outside a carriage window on a moving train.
By Juulia Ahvensalmi. This text was first published as 'Hysteria in the archives', St George's Library Blog, 28 Jan 2020.
Elizabeth Greed was 51 years old in 1888 when she was admitted to St George’s Hospital. Her medical case history, which survives in her post mortem record in the archives, tells us that she was married and had had five children; one of them had died. Another one was said to have tuberculosis, and one was said to be a ‘cripple’. When she was young she was said to have suffered from hysteria and scarlet fever.
Elizabeth herself said that about five years before, whilst walking in her garden, she had suddenly lost power in her legs. Although she recovered from this incident, she had been knocked down in the street the previous summer, and had struggled walking ever since. She also complained of various other ‘abnormal sensations’, including tingling in her limbs and a constricted feeling in her chest. She felt like she was floating in water when sat down, and when she walked, she could not feel the ground. She was also annoyed by a constant smell of sulphur.
She went to ask for treatment at Guy’s Hospital, but, feeling ill-treated there, took a cab to come to St George’s Hospital instead, then located at Hyde Park Corner. She was received by a young doctor called Richard Sisley, who in his notes describes her as ‘olive-skinned’ and her manner as ‘hysterical’. He says she only appeared to be able to walk supported, describing her movements resembling those of a marionette. He thought many of her symptoms pointed to hysteria, although the loss of power and the involuntary movements of her legs were suggestive of ataxic paraplegia – a condition that can be hereditary, or caused by damage to brain or the spinal cord, and is characterised by loss of motor function in the lower extremities.
 The post mortem record of Elizabeth Greed, Archives & Special Collections, St George’s, University of London, PM/1888/132
The post mortem record of Elizabeth Greed, Archives & Special Collections, St George’s, University of London, PM/1888/132
Elizabeth was admitted as an in-patient to the hospital on 7 March 1888. Further examinations found no abnormalities in her heart or lungs, but she was becoming increasingly paranoid and delirious. She thought she was being poisoned by turpentine mixed in her food. She was worried she would be sent out of the hospital, but she also thought that the ward she was in was filled with paraffin and would be set on fire. She lost weight, becoming increasingly weak, until she was unable to stand. On 11 April 1888, ‘she died without first symptoms, quietly’. The cause of death was recorded as possible mania and dementia, and ataxic paraplegia.
The case notes in the post mortem record of Elizabeth Greed do not elaborate more on her alleged hysteria, but her case gives us a glimpse of how women’s health was approached: despite her symptoms pointing to a physical condition, her behaviour is labelled as hysteric. Life in the 1880s London was not easy, and this was particularly the case for the poorer part of the population. We can assume that Elizabeth was poor, as those able to pay would not have attended a charitable hospital such as St George’s – they would have had the doctors come to them, or visited them at their private practices instead. The census records reveal that Elizabeth was from Clapton, and her husband Robert had moved to London from Taunton in Somerset. They lived in Bermondsey, which in the 19th century was a buzzing industrial hub, specialising in tanning, leather working, cotton work and food processing. All this industry meant that the population in Bermondsey was largely poor: the factories offered employment, but it was not particularly secure or well paid. Elizabeth is described as a ‘needlewoman’ (other related occupational terms include ‘dressmaker’ and ‘seamstress’). This was often work that could be done from home: sewing and mending clothes, making it easier for the women to care for their families. It was also, however, work that was very much underpaid, and the working conditions were likely to have been dire, with insufficient light and long hours, whether the work was done at home or in a factory.
But why was she labelled hysteric? Hysteria is no longer part of the medical vocabulary, but in the 19th century it was a common way to describe and diagnose what was perceived as emotional excess, primarily of women (this usage of course still continues outside medical diagnoses). It was seen to affect women from all social classes. The term encompassed a variety of symptoms, including anxiety, nervousness, agitation and demonstrations of sexual desire. Sexuality was at the heart of the condition; the word hysteria comes to English via Latin hystericus, from Greek ὑστερικός (husterikós, “suffering in the uterus, hysterical”), from ὑστέρα (hustéra, “womb”). Hysterical symptoms were thought to originate in the womb, and a commonly cited method of treatment was said to involve using a vibrator in order to gain release in the form of orgasm – this, however, is a myth rather than a commonly employed treatment.
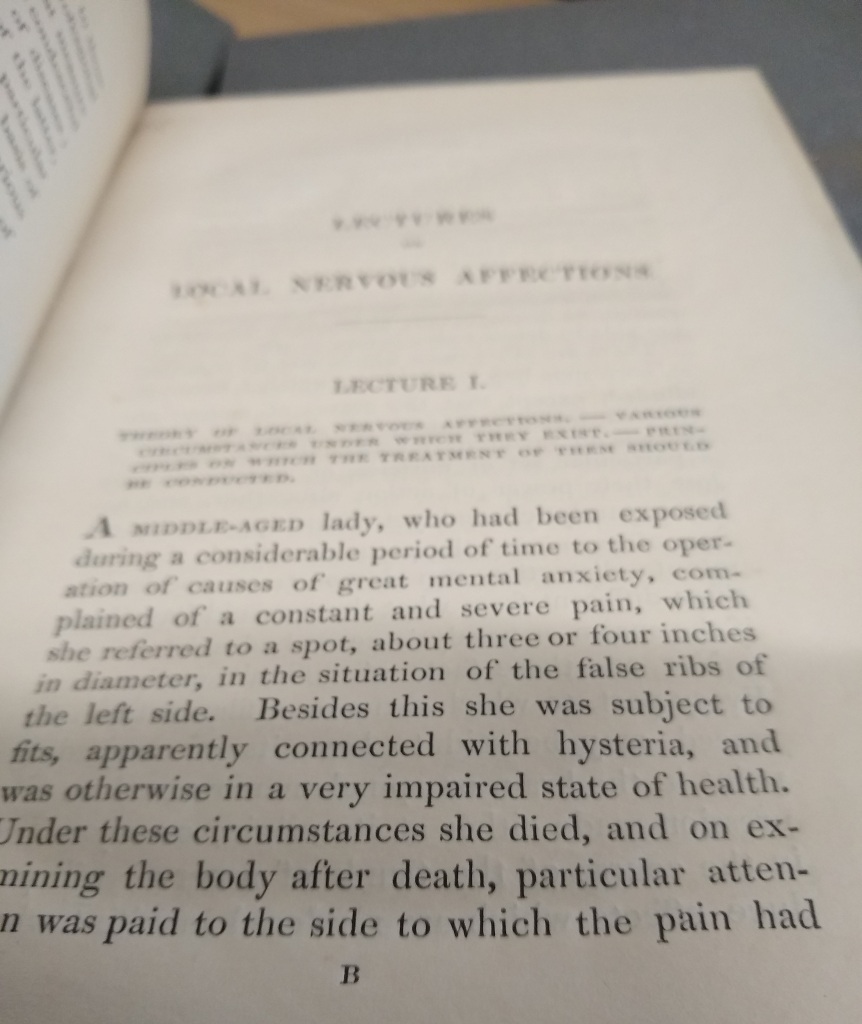 Brodie, Benjamin. 1837. Lectures Illustrative of Certain Local Nervous Affections. St George’s, University of London Archives. Credit: Juulia Ahvensalmi
Brodie, Benjamin. 1837. Lectures Illustrative of Certain Local Nervous Affections. St George’s, University of London Archives. Credit: Juulia Ahvensalmi
St George’s also plays a part in the history of hysteria. Benjamin Brodie, one of the most eminent doctors of his time and physician to the royal family, examined cases of ‘nervous affections’ in 1837. In these cases, patients had suffered from articular pain and swelling, but there had been no deterioration of bone or cartilage in the post mortem examination. In Brodie’s view these cases were neurological disorders, perhaps following a minor injury or a strong emotional experience, which could lead to a ‘hysterical knee’, for instance.
Another St George’s doctor writing about hysteria was Robert Brudenell Carter, who worked as an ophthalmologist at St George’s in 1870-1883. In his 1853 book ‘On the Pathology and Treatment of Hysteria’, he (unlike most of his contemporaries) emphasized the effect of emotions on the nervous system, arguing that a strong emotion might lead to a hysteric attack even in otherwise healthy women, as well as men. The prevalence of hysteria among women could, in his view, be explained by women’s heightened emotions, but also due to their having to suppress their emotions more than men, who were allowed to be physically and sexually more active.
The association of hysteria with the nervous system rather than the uterus, and with psychological, rather than physical, causes became more widely accepted during the 19th century. Jean-Martin Charcot was instrumental in re-defining hysteria in terms of neurological disorders, and his use of photography at the Salpêtrière asylum in Paris created controversial imagery of female hysteria.
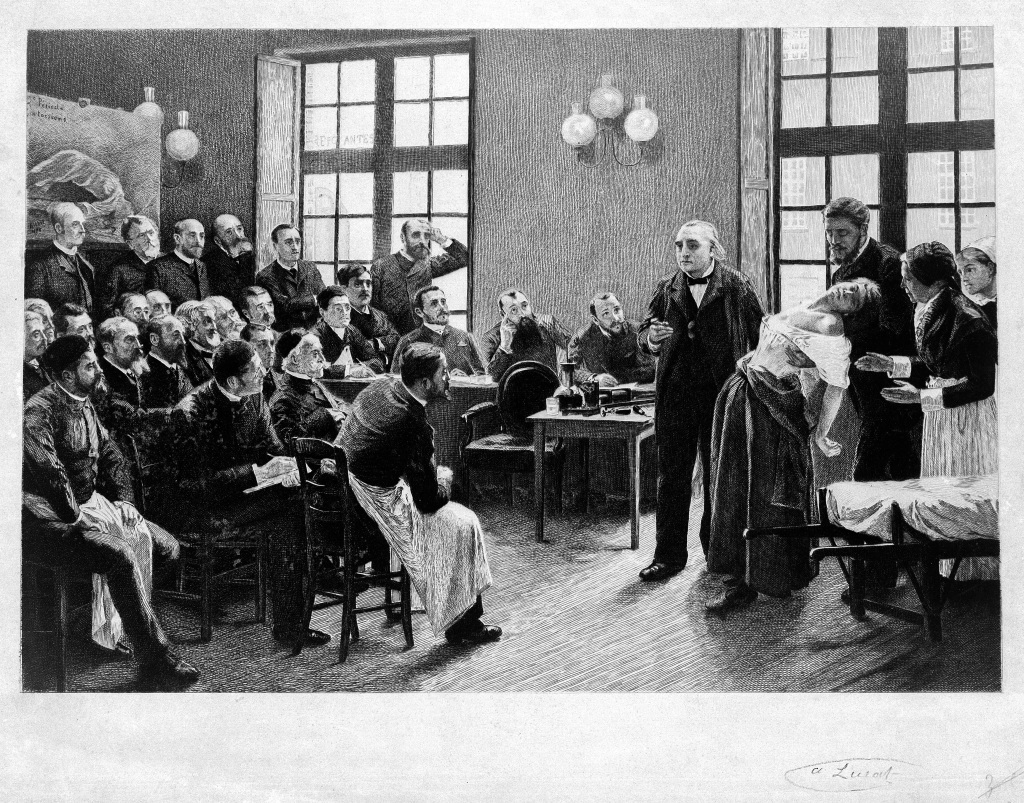 Jean-Martin Charcot demonstrating hysteria in a patient at the Salpetriere. Lithograph after P.A.A. Brouillet, 1887. Credit: Wellcome Collection. CC BY
Jean-Martin Charcot demonstrating hysteria in a patient at the Salpetriere. Lithograph after P.A.A. Brouillet, 1887. Credit: Wellcome Collection. CC BY
The American neurologist Silas Weir Mitchell advocated the so-called ‘rest-cure’ to calm the overstimulation of mind, which he believed was the cause of hysteria. This treatment was made infamous by Charlotte Perkins Gilman in her short story ‘The Yellow Wallpaper’ in 1891:
“John is a physician, and perhaps—(I would not say it to a living soul, of course, but this is dead paper and a great relief to my mind)—perhaps that is one reason I do not get well faster.
You see, he does not believe I am sick!
And what can one do?
If a physician of high standing, and one’s own husband, assures friends and relatives that there is really nothing the matter with one but temporary nervous depression—a slight hysterical tendency—what is one to do?
My brother is also a physician, and also of high standing, and he says the same thing.
So I take phosphates or phosphites—whichever it is, and tonics, and journeys, and air, and exercise, and am absolutely forbidden to “work” until I am well again.”
John W. Ogle, a physician at St George’s, discusses the case of Sarah G., 20, who was admitted to St George’s Hospital in 1869. She stated that she had been coughing and vomiting for about a year, and she had never menstruated until three weeks before her admission to the hospital. She had been treated previously at other hospitals for pain in the abdomen and vomiting. Ogle describes her as ‘rather delicate and interesting-looking’, and her manner as ‘somewhat sly and hysterical’.
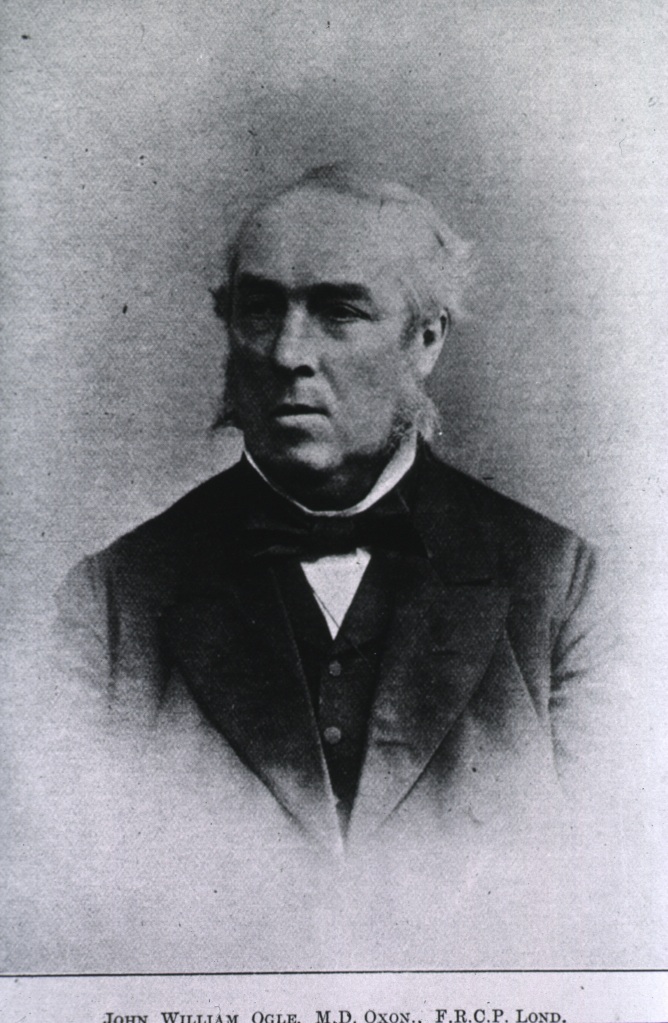 Caption: John William Ogle (1824-1905), physician at St George’s Hospital. Credit: US National Library of Medicine
Caption: John William Ogle (1824-1905), physician at St George’s Hospital. Credit: US National Library of Medicine
She was fed beef-tea and milk with limewater: beef broth was standard hospital fare, and the limewater was intended to relieve indigestion. Her constipation was treated with a ‘blue pill’ and the herbal remedies colocynth, senna draught and calumba; she was also given spirit of ammonia and bicarbonate of potassium. The so-called blue pill was (rather than Viagra!) a mercury-based medicine commonly used for this purpose, but also for treating a wide variety of other complaints, including syphilis, toothache and tuberculosis. Later various other medical concoctions were attempted, including calomel (mercury chloride), edemas made of castor oil and rue, belladonna (‘beautiful woman’ in Italian, from its cosmetic use for dilating pupils, the plant is also known as the deadly nightshade, and was used by the Roman empress Livia Drusilla to poison her husband emperor Augustus), brandy, prussic acid and morphine – it’s a wonder she was still alive at this stage, one might think!
Although her condition did not appear to be improving, she was seen to get up from her bed to watch Queen Victoria pass by the hospital on her way to open Blackfriars Bridge. This convinced Ogle that she must have been faking her illness. Despite her continued refusal to eat, she vomited and evacuated her bowels. Ogle quotes in his article a letter allegedly written by her to another patient, asking her to bring her a ‘nice peice [sic] of bread’ and to take care that she should not be seen to do so. She was further treated with faradisation (muscle stimulation by electric currents), and she was given daily baths until she got her period; she was also forced to do some exercise by walking her to the middle of the ward and then ‘leaving her to scramble back to her bed’. She appears to have got into disagreements both with the ward nurse and with Ogle, her doctor, until one day she suddenly walked out of the hospital.
Ogle diagnoses this case as ‘temper-disease’, suggesting that the original symptoms relating to her lungs may have been real enough to begin with, but that the attention received from exhibiting these symptoms had led the patient to feign further, imaginary, symptoms. He describes his patient as ‘by nature self-willed, with a ‘naughty’ disposition, badly trained, too well pleased to attract and receive attention, of an hysterical temperament’. Quoting Benjamin Brodie, he suggests that it is possible that even the cough was a hysterical symptom – a hysterical lung, if you will.
By Natasha Shillingford. This text was originally published as 'The pastry chef murderer', St George's Library Blog, 3 Sep 2020.
On 27th July 1908 a patient called Ferdinand Alletrie was admitted to St George’s Hospital with a stab wound in the left chest which was penetrating the heart. The medical case notes say that ‘He was a waiter at the Bath Club. He had quarrelled with a colleague who waited for him outside and stabbed him in the chest.’ On admission he was observed to be in articulo mortis, or at the point of death. There was a stab wound in the third left intercostal space just to the left of the sternum. His clothes were noted to be soaked in blood. Ferdinand died five minutes after his admission.
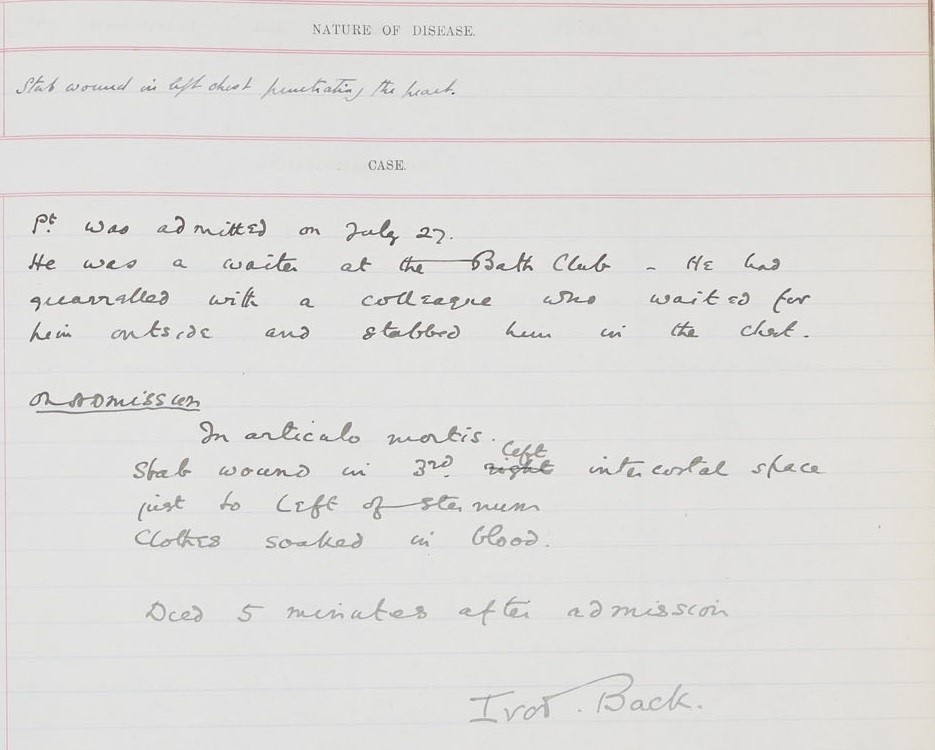 Post Mortem Case Book 1908 (Ferdinand Alletrie, PM/1908/221)
Post Mortem Case Book 1908 (Ferdinand Alletrie, PM/1908/221)
The morbid appearances listed during the post mortem examination note that on the left side of the chest in the third interspace was a ‘punctured wound pointed at either end and gaping in the middle. It measured 1” long and ½” wide in the middle.’ The Post Mortem includes an illustration of the murder weapon as shown below.
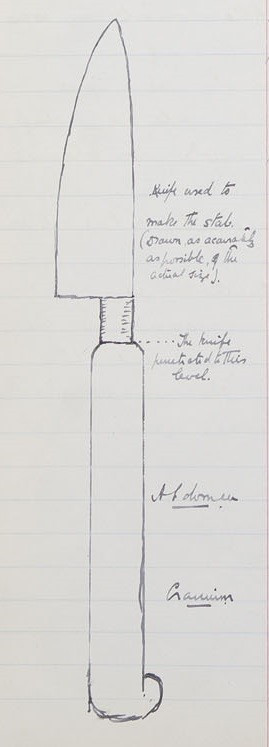 Post Mortem Case Book 1908 (Ferdinand Alletrie, PM/1908/221)
Post Mortem Case Book 1908 (Ferdinand Alletrie, PM/1908/221)
But what led to the death of Ferdinand at St George’s Hospital? A search through historic newspapers uncovered an article called ‘Foreigners’ Fight at the Bath Club’ in the Leicester Daily Post dated 1st August 1908. The article details the tragic events that took place at the Bath Club that evening as well as the resulting inquest at Westminster Coroner’s Court ‘on the body of a cook named Pierre Auguste Ferdinand Alletree, employed at the Bath Club, who died from the effects of a wound said to have been inflicted by another employee of the club, who was in consequences arrested.’ The accused man was named as Georges Backenstrass.
Pierre Souleyne, chef at the Bath Club, said that he had engaged Alletree as sauce cook at the beginning of June, and later employed Backenstrass as a pastry chef at the club. One evening Backenstrass approached the chef and said ‘Chef. I am very sorry. I want to leave at the end of the week.’ When asked why he wanted to leave, he said that he was not friendly with the sauce chef. Souleyne said to him, ‘You have nothing to do with the sauce cook, and he has nothing to do with you. You must work friendly together.’ The chef also spoke to the sauce cook, no doubt to diffuse the situation, and Alletree responded, ‘You know me. He is silly. Don’t take any notice of him.’ No doubt the chef thought the issue was resolved, but he soon received news that the two chefs were fighting.
Louis Ayrand, another sauce cook, gave evidence as to the relationship between the two chefs. He said that Backenstrass ‘was a quiet and reserved man. He had some malady, and for that reason he was avoided by the other men.’ He said that ‘we never ate any of his pastry’, because of this unnamed illness. Continuing, the witness said that Backenstrass and Alletree did not agree about their work, and they had previously quarrelled when Backenstrass would not send up the sauce. On the night of the murder Ayrand heard the two chefs quarrelling in the vegetable pantry, and they decided to settle matters outside in Berkeley Street. Soon another chef by the name of Griffin called out ‘The pastry cook has stabbed your chef.’ Soon after Alletree ran back to the club, his hand over his heart, pointed to the pastry chef and said ‘Arrest him, he has stabbed me with a knife.’
Griffin, a vegetable cook at the Bath Club, said that he had quarrelled with Backenstrass the same night, when he took a biscuit off the pastry chef’s plate and Backenstrass objected. Alletree then began arguing with Backenstrass, and the latter said ‘I will wait for you outside.’ Griffin followed the two men outside and saw Alletree put his hand to Backenstrass’ neck and push him back. Backenstrass retaliated by hitting Alletree in the chest with something, after which the sauce chef exclaimed ‘he has stabbed me.’
Another chef stated that he saw the cook with a knife after the quarrel and said to him ‘You ought not to use a knife when you have quarrelled.’ Backenstrass replied ‘Well, there are two waiting for me downstairs.’
When Backenstrass was taken to Marlborough Street Police Station he made a statement in which he said that the sauce cook had called him a sneak for talking to the chef about him, and that the sauce chef and Griffin had approached him in the pantry, the latter threatening to break his nose. Describing the affair in the street, Backenstrass said ‘I took my knife out of my right trousers pocket and struck him in the chest. The knife is very sharp. It is the one I used for pastry. I never carried it before that night. I took it because of the pastry cook and the vegetable cook. If they had left me alone this would not have happened. The sauce cook told me I had too many pans in the fire. He told me I ate too much and he would come and watch me out. I asked him several times to leave me alone, and he would not.’
Backenstrass was held at Brixton Prison prior to the inquest. However the Governor of the prison informed the Coroner that Backenstrass had committed suicide in prison by hanging himself in his cell. The Coroner pointed out to the Jury that although Alletree had started the quarrel, if Backenstrass was still alive they would have to commit him on the capital charge. The jury returned a verdict of wilful murder against Backenstrass.
A further search of the historic newspapers revealed the article ‘The Bath Club Tragedy. The Brixton Prison Suicide’ in the Faringdon Advertiser and Vale of the White Horse, 8th August 1908. The article discusses the inquest into the death of Backenstrass. A medical officer testified that the prisoner, apparently a German, had suffered from a nervous affection. There were marks of two wounds of an operation in the abdomen, ‘but the man was in fairly good health, and behaved himself quite rationally, though he shewed that he was naturally worried about the crime.’ On the prisoner’s slate was found words written to the effect that ‘he had not been in good health, that he felt the disgrace, that his conscience was quite clear, and that he was guiltless of the offence with which he was charged.’ The jury returned a verdict of suicide whilst of unsound mind.
By Natasha Shillingford. This text was first published as 'A case of leprosy in the archives', St George's Library Blog, 28 Feb 2020.
Natasha Shillingford, Project Archivist.
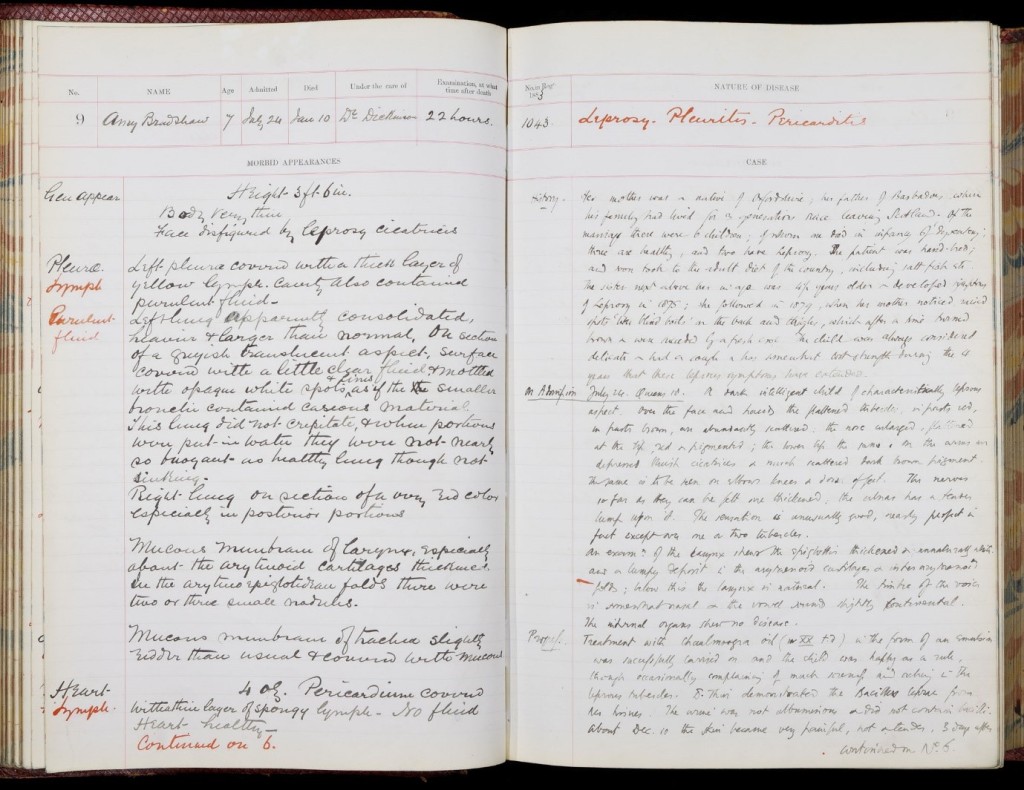 The post mortem record of Amy Bradshaw, Archives & Special Collections, St George’s, University of London, PM/1884/9
The post mortem record of Amy Bradshaw, Archives & Special Collections, St George’s, University of London, PM/1884/9
Amy Bradshaw, a seven-year-old girl, was admitted to St George’s Hospital on 24th July 1883 and she later died on 10th January 1884. She was suffering from Leprosy.
The medical case notes record that ‘Her mother was a native of Oxfordshire, her father of Barbados, where his family had lived for three generations since leaving Scotland.’ Amy was one of six children, one of whom died in infancy of dysentery, and two had Leprosy. The sister next above her in age was four and a half years older, and she developed symptoms of Leprosy in 1875. Amy was said to have first developed symptoms herself in 1879, when her mother noticed raised spots ‘like blind boils’ on her back and thighs, which after a time turned brown and were succeeded by a fresh crop.
On admission she was described as ‘a dark intelligent child of characteristically leprous aspect. Over the face and hand the flattened tubercles, in parts red, in parts brown, are abundantly scattered: the nose enlarged, flattened at the tip, red and pigmented; the lower lip the same.’ On her arms, legs and feet were depressed cicatrices and scattered dark brown pigment.
On examination the larynx and epiglottis were found to be thickened and unnaturally white and a lumpy deposit was found. ‘The timbre of the voice is somewhat nasal and the vowel sounds slightly continental.’
Amy was treated with Chaulmoogra Oil in the form of an emulsion which was seen as a success and the child was happy as a rule, although she occasionally complained of soreness and aching in the leprous tubercles. On 17th December her temperature rose rapidly ‘when an acute invasion of the new growth set in with much pain and suppuration.’ The medical case notes report that Amy’s elder sister who was suffering from the same symptoms, was allowed to leave the hospital on 23rd December to spend Christmas at home. However, she developed pneumonia shortly after and died on 6th January. Amy also gradually developed pneumonia in the hospital and ‘sank with great pain, and high fever, dying in Jan 10 1884.’ The post mortem report states ‘Face disfigured by leprosy cicatrices.’
Leprosy affects the nerves, respiratory tract, skin and eyes. It can cause loss of fingers and toes, gangrene, ulcerations, skin lesions and weakening of the skeleton. If left untreated, it can lead to a loss of sensation in the hands and feet. This lack of ability to feel pain can lead to the loss of extremities from repeated injuries or infection due to unnoticed wounds. Leprosy can also damage the nerves in the face which causes problems with blinking and eventual blindness. Other symptoms, which can be seen in the case of Amy Bradshaw, include flattening of the nose due to destruction of nasal cartilage, and phonation and resonation of sound during speech.
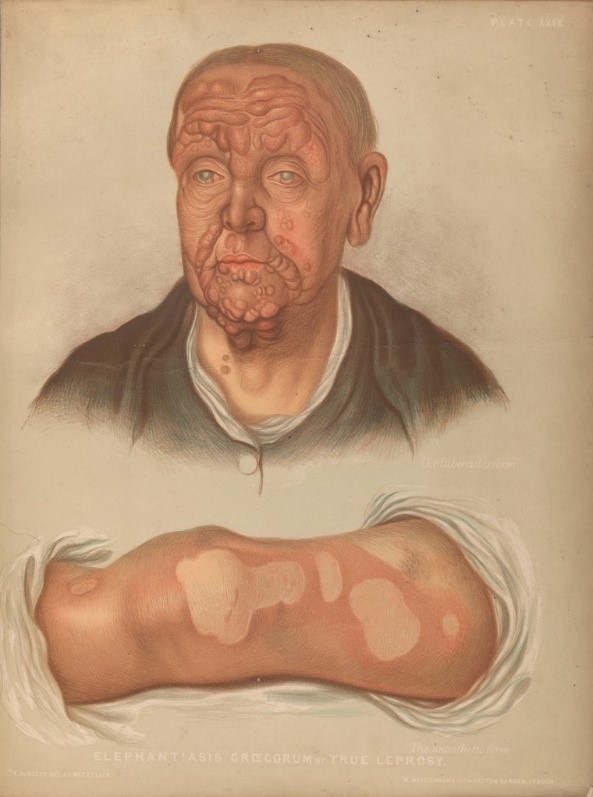 Credit: Elephantiasis graecorum, True Leprosy. Chromolithograph.
Credit: Elephantiasis graecorum, True Leprosy. Chromolithograph.
Credit: Wellcome Collection. Attribution 4.0 International (CC BY 4.0)
The disease takes its name from the Greek word λέπρᾱ (léprā), from λεπῐ́ς (lepís; “scale”). Leprosy has a long and complicated history and for centuries has been associated with social stigma, which even in the modern day continues to be a barrier to self-reporting and early treatment.
The earliest possible account of a disease which is believed to be Leprosy appears in an Egyptian papyrus document written around 1500 BC. Indian texts from 600 BC also describe a disease that resembles Leprosy. The first account of the disease in Europe occurs in the records of Ancient Greece after the army of Alexander the Great came back from India, and then in Rome in 62BC which coincided with the return of troops from Asia Minor.
Leprosy had entered England by the 4th century AD and was a common feature of life by 1050, although throughout its history it has been feared and misunderstood. It was often believed to be a hereditary disease, or some believed that it was a punishment or curse from God. Pope Gregory the Great (540-604) considered people with Leprosy to be heretics.
Others thought that the suffering of lepers echoed the suffering of Christ and they were enduring purgatory on earth and would go straight to heaven when they died. Therefore, they were considered closer to God than other people.
Leprosy patients were often stigmatised and shunned by the rest of society. During the middle ages people suffering from Leprosy were made to wear special clothing, ring bells to warn others of their presence, and walk on a different side of the road.
 Credit: Manuscript showing leper. Credit: Wellcome Collection. Attribution 4.0 International (CC BY 4.0)
Credit: Manuscript showing leper. Credit: Wellcome Collection. Attribution 4.0 International (CC BY 4.0)
A passage from Leviticus 13: 44-46 shows the biblical perception that people with leprosy were unclean and should be ostracised from society:
the man is diseased and is unclean. The priest shall pronounce him unclean because of the sore on his head.
Anyone with such a defiling disease must wear torn clothes, let their hair be unkempt, cover the lower part of their face and cry out, ‘Unclean! Unclean!’ As long as they have the disease they remain unclean. They must live alone; they must live outside the camp.
 Credit: Two lepers receiving food through a wall. Etching by Gaitt after A. Decamps. Credit: Wellcome Collection. Attribution 4.0 International (CC BY 4.0)
Credit: Two lepers receiving food through a wall. Etching by Gaitt after A. Decamps. Credit: Wellcome Collection. Attribution 4.0 International (CC BY 4.0)
Even in more modern times, patients with Leprosy were often confined to colonies called Leprosariums because of the stigma of the disease. Some of these colonies were situated in remote lands or islands, such as the island of Spinalonga off the coast of Crete which was used as a leper colony from 1903 to 1957. The novel ‘The Island’ by Victoria Hislop tells the story of the leper colony on Spinalonga and its inhabitants.
In 1873 Dr Gerhard Henrik Armauer from Norway identified the germ that causes Leprosy. The discovery of Mycobacterium Leprae proved that leprosy was not a hereditary disease, or a punishment by God, but an infection caused by bacteria.
Patients with Leprosy were often treated, as can be seen in the case of Amy Bradshaw, with oil from the chaulmoogra nut. The treatment was said to be painful and its success was questionable, although some patients appeared to benefit. Leprosy is now curable with multidrug therapy (MDT) which was developed in the early 1980s
The last case of indigenous leprosy in the UK was diagnosed in 1798. Leprosy can no longer be contracted in this country, but there are around 12 new cases diagnosed each year. The World Health Organisation (WHO) (https://www.who.int/news-room/fact-sheets/detail/leprosy) figures state that in 2018 there were 208,619 new cases of leprosy diagnosed. This is approximately one every two minutes.
By Juulia Ahvensalmi. This text was originally published as 'Nothing new under the sun: 1870s style contact tracing and smallpox vaccinations', St George's Library Blog, 31 Mar 2021
‘It is difficult to imagine a more favourable opportunity than the one recently afforded us here, of investigating the laws of an epidemic disease such as the one we have just experienced’
Thomas Jones, ‘On the Recent Outbreak of Smallpox at St George’s Hospital’ (1870)
‘Contact tracing’ has in the past year become a phrase that is surely now familiar to us all. As a concept, however, it’s nothing new. In this blogpost, we’ll take a look at how St George’s reacted to a smallpox epidemic at the hospital.
In November 1870, smallpox cases started spreading within St George’s hospital. The infected patients had all been admitted for other causes, and had all been in the hospital for a long time – somewhere between two weeks and four months. It seemed clear the disease was being somehow transmitted among the patients, but as the cases occurred in different wards and floors with no direct contact between the patients, the route of transmission was a mystery.
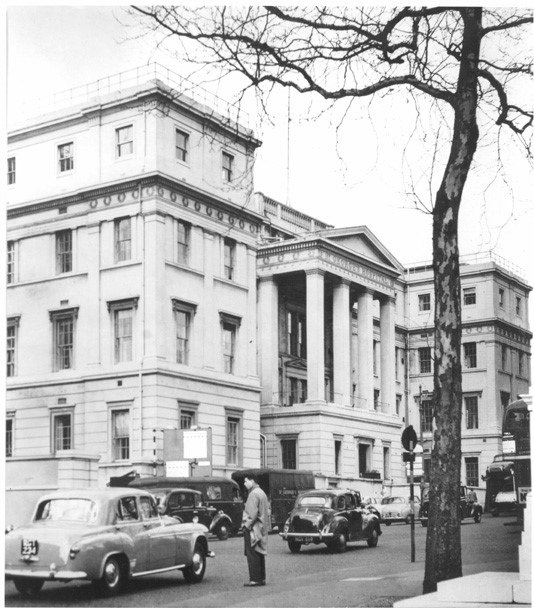 Image 1. St George’s Hospital at Hyde Park Corner, London. Archives and Special Collections, St George’s, University of London.
Image 1. St George’s Hospital at Hyde Park Corner, London. Archives and Special Collections, St George’s, University of London.
Generally, patients with infectious diseases were sent to specialised hospitals to prevent the spread in more general hospitals. Two of these so-called fever hospitals were the Fountain Hospital and the Grove Hospital, which stood side by side on the site now occupied by St George’s in Tooting. The Fountain Hospital was established by the Metropolitan Asylums Board (MAB) in 1893 in response to a scarlet fever epidemic, and later became a mental hospital for children. The Grove Fever Hospital opened in 1899; in 1954 it became the Tooting branch of St George’s. The last remaining buildings are now being demolished.
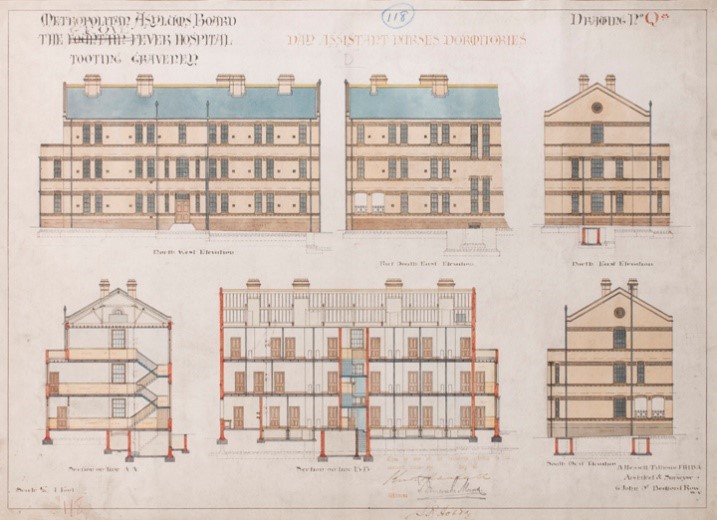 Image 2. Architectural drawing showing ‘The Fountain Grove Fever Hospital, Tooting Graveney’. Archives and Special Collections, St George’s, University of London.
Image 2. Architectural drawing showing ‘The Fountain Grove Fever Hospital, Tooting Graveney’. Archives and Special Collections, St George’s, University of London.
 Image 3. An aerial view of St George’s site with Fountain and Grove Hospitals in the 1930s, and a view of the final buildings being demolished on a grey day in March 2021. Archives and Special Collections, St George’s, University of London.
Image 3. An aerial view of St George’s site with Fountain and Grove Hospitals in the 1930s, and a view of the final buildings being demolished on a grey day in March 2021. Archives and Special Collections, St George’s, University of London.
Tracing the epidemic
Sarah M., 23, was admitted into St George’s hospital on 28 Sep 1870 for ‘syphilitic laryngitis’. For several weeks, she was given potassium iodide. The first smallpox eruptions appeared nearly two months after her initial admission, and were first thought to be a side effect of her medication. When her condition became apparent, she was quarantined in a separate room in the basement of the hospital, her bed and bedlinen were disinfected, and she was moved back to the workhouse she had come from only a few days later (which sounds like not very effective quarantine practice, but we’ll come back to that later).
Thomas Jones, MD, wrote an article on the outbreak in St George’s Hospital and Medical School Annual Reports, which consisted not only of reports of specifically relating to St George’s (despite the name), but also of articles by the staff of St George’s and external contributors. These were printed and widely distributed, and have been digitised by HathiTrust from copies held at Harvard University and University of Michigan: we are very grateful for this, especially now when our access to our own physical archives remains sporadic! Jones had only gained his MD earlier that year from St George’s, and was working at the hospital as resident medical officer and anaesthetist.
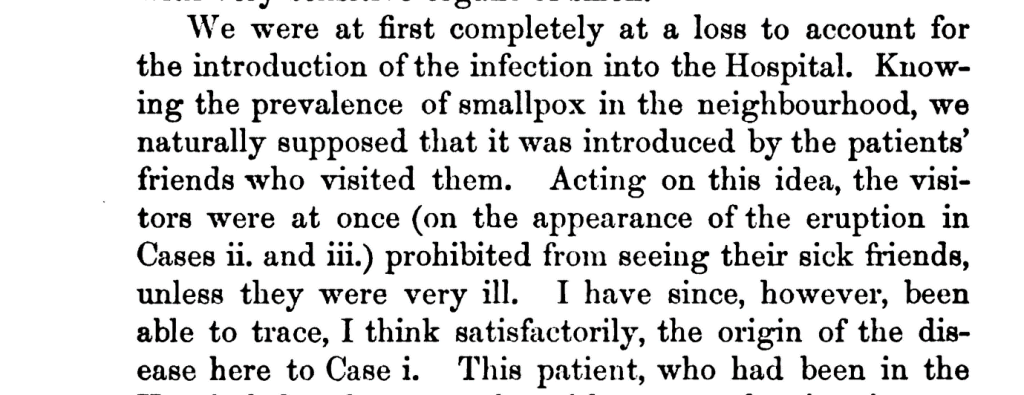 Image 4. Thomas Jones, ‘On the Recent Outbreak of Smallpox at St George’s Hospital’ (1870). St George’s Hospital reports, vol. 5 (1870). Full text available via HathiTrust and SGHMS/6/1/5, Archives and Special Collections, St George’s, University of London.
Image 4. Thomas Jones, ‘On the Recent Outbreak of Smallpox at St George’s Hospital’ (1870). St George’s Hospital reports, vol. 5 (1870). Full text available via HathiTrust and SGHMS/6/1/5, Archives and Special Collections, St George’s, University of London.
The article details the cases of the infected patients, with remarks on whether the patient in question had been vaccinated:
‘CASE XV. Mary H., æt. 12, admitted December 12, Drummond Ward. Suffering from knocked-knees. Smallpox eruption, very modified, appeared on January 9th. Discharged convalescent, January 31st. Vaccinated in infancy; vaccine cicatrices of excelled quality.’
‘Case XIX. Florence B., æt.19, admitted December 14th, Crayle Ward. Eczema. Smallpox eruption, which was distinct, appeared on January 14th. Was re-vaccinated on the same day. The attack was rather severe. There was no trace of the re-vaccination on the seventh day. Was vaccinated in infancy; one vaccine mark of bad quality. Has made a good recovery.’
There were altogether 27 cases, of which 20 were cases of transmission within the hospital, whose symptoms appeared between 25 Nov and 15 Jan. In addition, there were three patients who were admitted with smallpox between 12 Jan and 8 Feb, and four who showed symptoms only after having been discharged from the hospital initially.
Post mortems
Of these 27, six died. They were all said to have been suffering from various underlying conditions, including softening of the spinal cord, heart disease, pyelitis and congested lungs; one was recovering from an operation and one, a 23-year old probationer nurse at St George’s called Christiana S. in the article, was said to be ‘of a delicate constitution’ and in ‘a weak state of health’. Three of these six had been vaccinated.
The death of Christiana S., or Christina Stewart, was recorded in the St George’s post mortem books, although there are no case notes as no post mortem was performed – not uncommon when it came to hospital staff. Her cause of death is recorded as ‘Variola’, another name for smallpox.
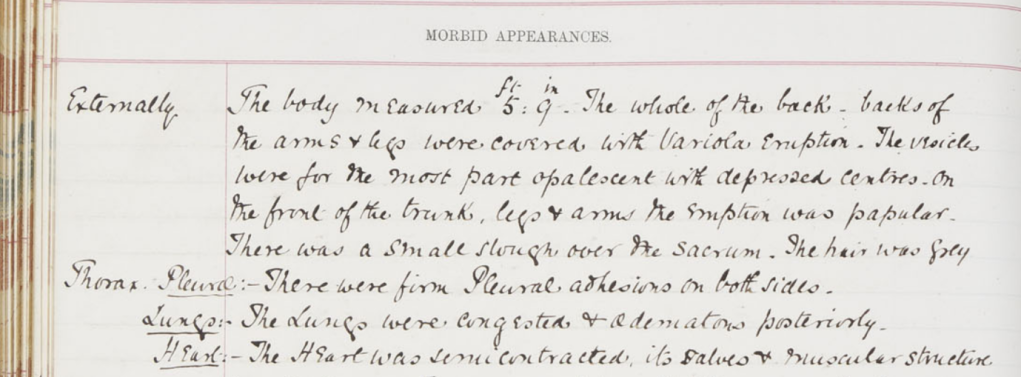 Image 5. Post mortem case notes of James Jennings, 37, Pork butcher, PM/1871/12. Archives and Special Collections, St George’s, University of London.
Image 5. Post mortem case notes of James Jennings, 37, Pork butcher, PM/1871/12. Archives and Special Collections, St George’s, University of London.
One of the unfortunate people who died was James Jennings. His occupation in his post mortem notes was recorded as ‘pork butcher’, and he had been suffering from a feeling of tightness around his abdomen and increasing weakness in his legs for some time; he was also partially paralysed on his hands and legs:
‘He walked to the train on day of admission but says that while in the carriage he felt a sudden sensation of coldness all over, & on reaching London found that he had entirely lost power in the legs’
His treatment included potassium iodide and belladonna. The rash appearing on his skin was initially attributed to the belladonna he had been receiving, rather than smallpox. He died 8 Jan 1871, a couple of days after the appearance of the pustules signifying a smallpox infection, ‘in spite of wine, which was freely administered’. The post mortem found no evidence that he had been vaccinated against smallpox.
The other deaths recorded include that of Ellen Collier, a milliner (whose body was not examined) and David Edwards, a groom, who became delirious and died after being moved to the temporary smallpox ward which had been set up on the top floor of the hospital.
The two other deaths occurred outside the hospital, and are not recorded in the post mortems. Michael S., 48, had been discharged from the hospital 28 Dec; he had spent the following night at Vauxhall-bridge-road, before returning home to Fellday, Dorking. He died 12 Jan 1871, and was examined by a local doctor in Dorking. John T. was only three years old, and had had lithotomy performed on him. Whilst at the hospital, he developed a sore throat, which was assumed to be due to ‘hospital air’ and was sent home, where he died less than a week after the appearance of the smallpox pustules. He had not been vaccinated.
Prevention and tracing the origins of the epidemic
The measures taken at the hospital to mitigate the spread of the disease included isolation of the infected patients: after the first three cases, a convalescent ward on the top floor was set up as a smallpox unit. The ward had dedicated nurses, and no visitors were allowed: the medical officer in charge visited this ward after all his other rounds. Particular attention was also paid to disinfecting the hospital:
‘For the atmosphere of the whole Hospital has been so thoroughly impregnated with carbolic acid, from sheets steeped in it and hung before the door of each ward, and from the floors being washed with a weak solution of the acid, that it has positively been painful to some with very sensitive organs of smell.’
The initial assumption was that the disease had been brought in by visitors, as it was known that smallpox was circulating in the neighbourhood, having, according to the Medical Officer of Health report, been introduced by a governess returning from Paris. Visitors were therefore banned from the wards, unless there were special reasons, i.e. the patient they were visiting was very ill.
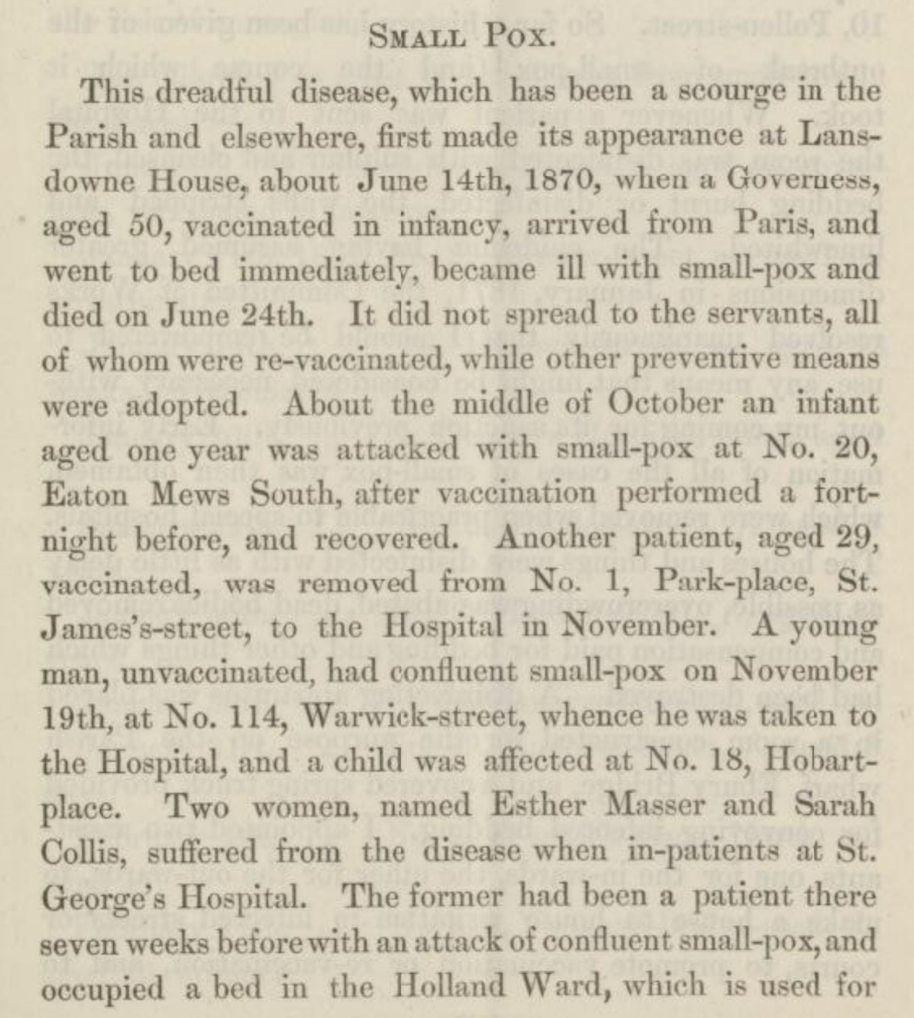 Image 6. Report of the Medical Officer of Health for Hanover Square, The Vestry of the Parish of Saint George (1871). Available via ‘London’s Pulse: Medical Officer of Health reports 1848-1972’ Wellcome Library.
Image 6. Report of the Medical Officer of Health for Hanover Square, The Vestry of the Parish of Saint George (1871). Available via ‘London’s Pulse: Medical Officer of Health reports 1848-1972’ Wellcome Library.
Jones set up to detect the origin of the disease. Assuming the incubation period to be 13×24 hours (or 14 days), from the infection to the appearance of an eruption, he managed to trace patient zero, or Case I, Sarah M., who had spent 11 weeks at the hospital.
On 10 Nov, however, she had been allowed to leave the hospital for a few hours to visit a friend, who was later ascertained to have smallpox. Sarah had, however, since been moved back to the workhouse (there is no note in the article of whether the workhouse also suffered from an outbreak, but it is hard to imagine it did not), and Cases II and III did not appear until three weeks later, on a different floor – so how was it possible that the disease continued to spread at the hospital? Moreover, the cases continued to spread even after the visitor ban and the ‘rigidly observed’ quarantine measures.
Did it spread through the air? This theory was dismissed as unlikely, since the cases were so spread over different floors and wards. All other theories were similarly dismissed, and after careful investigation, the only common factor between the cases appeared to be the days when bed-linen was changed.
The linen was changed on Mondays and Thursdays: the dirty linen was sent out to be washed on Thursdays and returned, clean, the following Thursday. One sheet was used on that day, and another clean sheet on the following Monday. This theory seemed to account for the majority of the cases, with a few exceptions, one of which included the hospital carpenter, who may instead have caught the disease through contact with one of the patients.
This led to Jones concluding that the disease was infectious even before any eruptions appeared, and thus any cases of fever during an epidemic should be closely monitored to enable early isolation and disinfection.
Linen was supposed to be washed in boiling water, but, whether or not that actually happened (and washing the linen for the hospital was not an easy or light task!) this, it was concluded, was ‘not sufficient to destroy the fever-poison’. Carbolic acid, however, appears to have worked, as the sheets of the patients known to be infected were steeped in carbolic acid before being sent to the laundry.
 Image 7. Nurses in the laundry of a hospital. Photograph, 191-.. Credit: Wellcome Collection. Attribution 4.0 International (CC BY 4.0)
Image 7. Nurses in the laundry of a hospital. Photograph, 191-.. Credit: Wellcome Collection. Attribution 4.0 International (CC BY 4.0)
Vaccination
The main conclusion, however, was to do with vaccination, and in particular re-vaccination:
‘This outbreak … supplies us with farther evidence, if any were required, of the protective power of re-vaccination against smallpox’
Indeed, as the disease spread, it was decided that all the nurses and patients at the hospital should immediately be vaccinated. The vaccination programme was commenced on 13 January 1871, and by March, the measures taken appeared to have stopped the spread of the epidemic.
A follow-up article by obstetric assistant Richard Wilson examines how the vaccination programme was conducted. Three methods were used:
- Puncturing: ‘by grasping the arm (usually the left) with the left hand, drawing the skin tense, and then making from four to five punctures down to the cutis-vera with an arrow-headed lancet’;
- Abrasion or scratching, using an ‘ordinary bleeding-lancet’: ‘two or three small parallel scratches were made …. the lymph, if liquid, was then rubbed well in with the point of the lancet; if points were used, these were first moistened by the breath, and rubbed into the different scratches’; and
- Vesication, using ‘blistering fluid’ the night before the vaccination to make small blisters: ‘on the following day they were priced to allow the serum to exude, and then the lymph was applied to the raw surface’.
The scratching method appeared to be most effective, although it was prone to produce severe inflammation in the elderly or those with other health conditions.
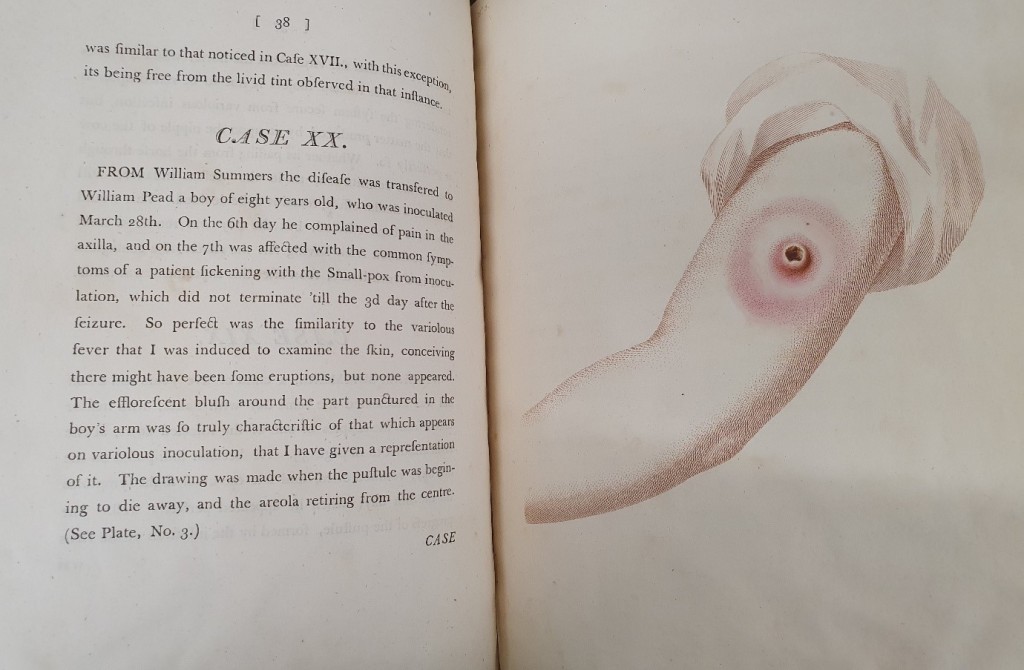 Image 8. Edward Jenner, ‘Causes and Effects of Variolae Vaccinae’ (1798), showing the effect of inoculation against smallpox. RB/285, Archives and Special Collections, St George’s, University of London.
Image 8. Edward Jenner, ‘Causes and Effects of Variolae Vaccinae’ (1798), showing the effect of inoculation against smallpox. RB/285, Archives and Special Collections, St George’s, University of London.
The quality of the ‘vaccine marks’ or ‘cicatrices’ appears of particular interest, with ‘good marks’ equating, it was speculated, to stronger protection and increasing the likelihood of a mild form of the disease. ‘Bad’ marks were smooth and shiny, or hardly visible at all: the stronger and more visible the mark, it was thought, the stronger the protection. The vast majority of the staff and patients had already been vaccinated at some point in their lives, most of them in infancy.
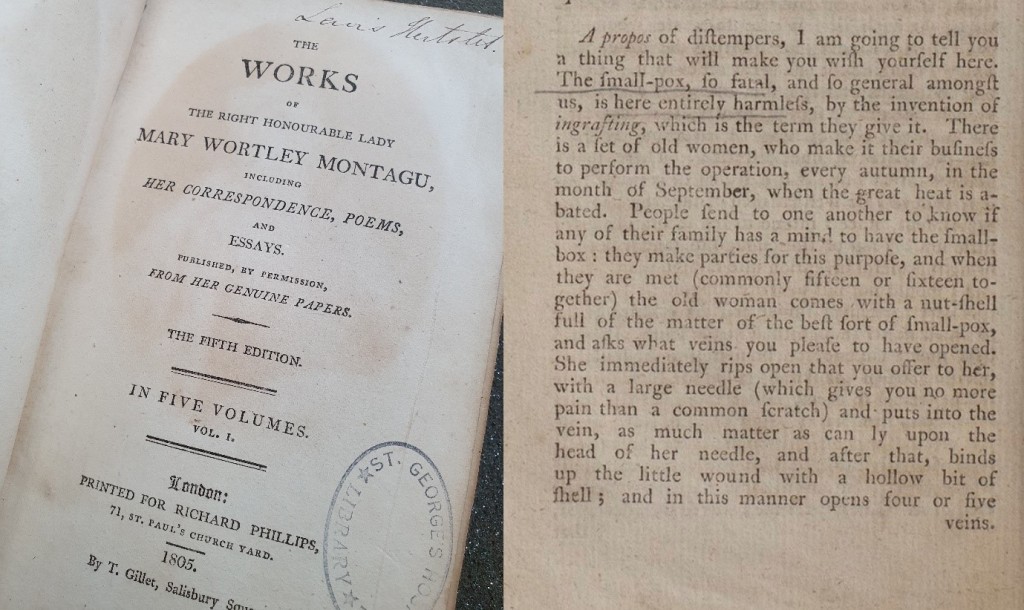 Image 9. Montagu, Mary Wortley. ‘The Works of the Right Honourable Lady Mary Wortley Montagu’ (1805 [1785]), with a description of a ‘smallpox party’ in Istanbul. RB/317, Archives and Special Collections, St George’s, University of London.
Image 9. Montagu, Mary Wortley. ‘The Works of the Right Honourable Lady Mary Wortley Montagu’ (1805 [1785]), with a description of a ‘smallpox party’ in Istanbul. RB/317, Archives and Special Collections, St George’s, University of London.
Smallpox epidemics were common throughout the 19th century, despite Edward Jenner, a St George’s alumnus, having developed smallpox vaccination in 1796. He was not the first one to attempt to treat the disease, one of the deadliest in history. Mary Montagu introduced the idea of inoculation from Turkey to Britain in the early 1700s. Smallpox was not eradicated until 1973, and to date remains the only human disease to have been eradicated by vaccination.
Read the full case notes here.
Martin Cahill, a groom by occupation, was bitten on his wrist by a harrier (a dog breed associated with hare hunting) in 1887. The kennel where the dog came from was known to have rabies; alarming news, as the symptoms of rabies, also known as hydrophobia ('fear of water'), include violent movements, paralysis and confusion, and are almost inevitably fatal.
In the 1880s there was, however, some hope of recovery: Louis Pasteur, the French chemist and microbiologist who gave his name to the process of pasteurization, had developed vaccine against rabies with Émile Roux only two years before, in 1885. Word about the new treatment spread quickly, and people travelled from all over the world to Pasteur's clinic (and, later, to the Pasteur Institute) in Paris to be vaccinated.
The medical notes accompanying Cahill's post mortem record note that 'he went to Paris & was there treated by the Pasteur inoculation system, after the original wound had been excised. Eight or 10 inoculations were made on the abdomen. He returned from Paris about Aug 20, & came up as OP [out-patient] with the wound unhealed’. Although the success rates were reported to be very high, this was unfortunately not the case for Cahill, who died at St George's Hospital in Hyde Park Corner in August 1887. Perhaps he, however, contributed to the scientific understanding of the disease, as the post mortem notes that his brain was reserved for 'microscopical examinations'.
By Juulia Ahvensalmi. This text was originally published as 'Digits: For Good': Vaccinating Harrods and Selfridges, or, (Digital) preservation of COVID-19 and influenza records', St George's Library Blog, 5 Nov 2020.
Digital Preservation Day 2020 celebrates the positive impact of digital preservation. The theme ‘Digits: For Good’ focuses this year on the creation and preservation of research and development data used in finding a vaccine for COVID-19. In this post we’ll look into the work we’ve been doing to preserve these records, and also what the archives can tell us of past pandemics. This blogpost has been written by St George’s Archivist Juulia Ahvensalmi, Records Manager Kirsten Hylan and Research Data Support Manager Michelle Harricharan. You can engage with the day and find out more about our work on Twitter at @CollectionsSgul and @sgullibrary and using the hashtags #WDPD2020 and #SGULWDPD2020.
Our COVID-19 story
At St George’s, University of London (SGUL), a specialist health and medical sciences university in South-West London, the Archivist, Research Data Support Manager, and Records Manager have joined forces to advocate for digital preservation.
When it comes to meeting the challenge of preserving our digital materials, we have found that by bringing together staff members from different areas of the University we can utilise different skills and internal networks to achieve our goals.
As part of the work we are undertaking around digital preservation, the team aims to collect all Covid-19 related material produced by SGUL. This includes a variety of documents in a variety of formats, produced by different parts of the university, including
- Communications, such as emails, web pages, FAQs, video recordings and social media. These provide evidence of our response to the crisis and our management of it – something that will be both interesting and important to keep for the future. Communications sent out to students, staff, alumni as well as those externally available will tell the story of how St George’s reacted to the pandemic
- Governance records, including minutes of meetings. These provide evidence of the conversations and decision-making about the responses and management of the pandemic
- Research, including recording the range of Covid-19 research St George’s researchers have been involved in throughout the pandemic as well as our researchers’ incredible work in the national and international media. Research data from these studies are also important to collect and preserve for the long term.
To date we are curating and preserving the items that we aware of, and we have started conversations with departments such as External Relations, Communications and Marketing to identify material we may have missed.
We are conscious of the need to collect the full complement of Covid-19 material as ultimately this material will be an important part of our Archive in years to come and support future research.
Looking back
The majority of the material related to COVID-19 is digital, but that is not the case for most of the material held in the archives (although in the future that is of course likely to change!). The one pandemic most often compared to COVID-19 is the 1918-1919 influenza pandemic, known most commonly (and misleadingly) as the ‘Spanish’ flu, or ‘the Grippe’. Estimates of the number of deaths caused by it vary anywhere from 17 to 100 million people worldwide.
In order to understand more about the current pandemic, and our responses to it, and to learn from our past mistakes, we need to look into the past. How did St George’s, then, respond to this pandemic? Well – the answer is that we don’t really know. The minutes of the Medical School (later SGUL) committee and council make no reference to the pandemic. St George’s Hospital and Medical School Gazette, journal produced by St George’s staff and students between 1892 and 1974, notes in February 1919 that the out-patient department and many wards at the hospital had to be closed as so many nurses were off sick, but the medical school records don’t reveal much more (although St George’s Hospital records, which are held at the London Metropolitan Archives, may hold more information).
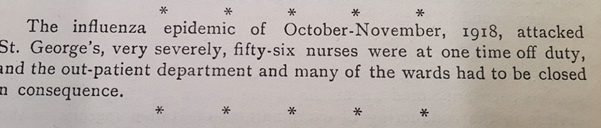 St George’s Hospital and Medical School Gazette, Feb 1919. Archives and Special Collections, St George’s, University of London.
St George’s Hospital and Medical School Gazette, Feb 1919. Archives and Special Collections, St George’s, University of London.
What we do have is historical post mortem examination records, which we are currently cataloguing and making available online. These records provide an incredible source for studying death and disease in 19th and early 20th century London. They chart, among other things, the 1854 cholera epidemic, show how prevalent tuberculosis was, and contain numerous fascinating and illuminating cases, such as that of the pastry chef murderer in 1908.
 Post mortem and case book 1846, PM/1846. Archives and Special Collections, St George’s, University of London.
Post mortem and case book 1846, PM/1846. Archives and Special Collections, St George’s, University of London.
When we started cataloguing the volumes for 1918 and 1919, we were expecting to find plenty of examples of influenza, and were surprised when, well, there just weren’t that many.
There were, of course, some cases, and many that sound troubling, such as the case of Ada Bell, a soldier’s wife aged 32, who died at St George’s 31 Oct 1918. Her illness was initially diagnosed as pneumonia, but she was brought to the hospital delirious, coughing and suffering from diarrhoea, deafness and shortness of breath. Her cause of death was deemed to be typhoid fever and influenzal bronchopneumonia.
![Scan of Post mortem case of Ada Bell, [Wife of] Soldier, 32, PM/1918/240. Archives and Special Collections, St George’s, University of London.](/image-library/default-images/image31.jpg) Post mortem case of Ada Bell, [Wife of] Soldier, 32, PM/1918/240. Archives and Special Collections, St George’s, University of London.
Post mortem case of Ada Bell, [Wife of] Soldier, 32, PM/1918/240. Archives and Special Collections, St George’s, University of London.
As the symptoms were varied, cases were sometimes misdiagnosed as dengue, cholera or typhoid, for instance. Of the overall deaths in those two years at St George’s, influenza cases account for 5.5% of all the cases: the yellow line in the graph below shows cases where influenza was reported to be the cause of death (or, to be more specific, cases in which influenza is mentioned in the post mortem report). We don’t, however, have the admissions registers for the hospitals, so we cannot tell the number of cases overall, only the number of deaths.
There is a relatively large number of ‘unknown’ causes of death during these years as well (shown in turquoise in the graph below) – these are cases for which the records enter no cause of death and no details on the medical case, and they may or may not include some further influenza cases. The graph also shows other respiratory tract diseases (in green) and digestive system diseases (in purple).
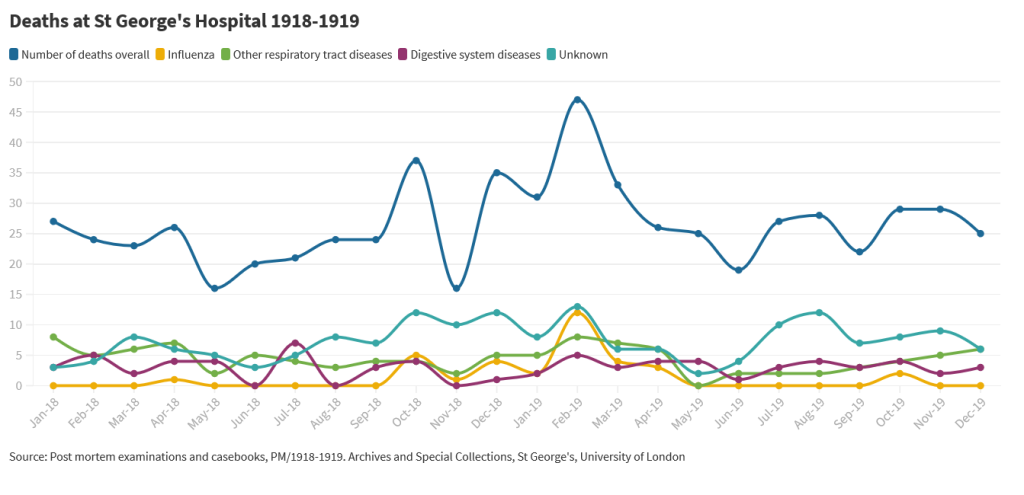 Deaths at St George’s Hospital 1918-1919. Source: Post mortem examinations and casebooks, PM, Archives and Special Collections, St George’s, University of London.
Deaths at St George’s Hospital 1918-1919. Source: Post mortem examinations and casebooks, PM, Archives and Special Collections, St George’s, University of London.
The 1889 influenza
Influenza was of course not confined to these years only. Every so often influenza cases would flare up, and the previous time this happened on a large scale in 1889-90. With our propensity for blaming single countries for viruses, this pandemic is sometimes referred to as Russian flu and, according to some theories, it may have played a part in immunising those who had it against the 1918 flu, which appeared to disproportionately strike the younger population.
There were attempts at finding medicines to cure the disease, and there was a minor scandal when the name of the teacher of materia medica (the study of drugs to treat diseases) at St George’s was found printed on an advertisement for an influenza cure: despite denying his involvement, he had to resign. The advertisement does not actually tell us what the medication consisted of, but we can only assume it did not work.
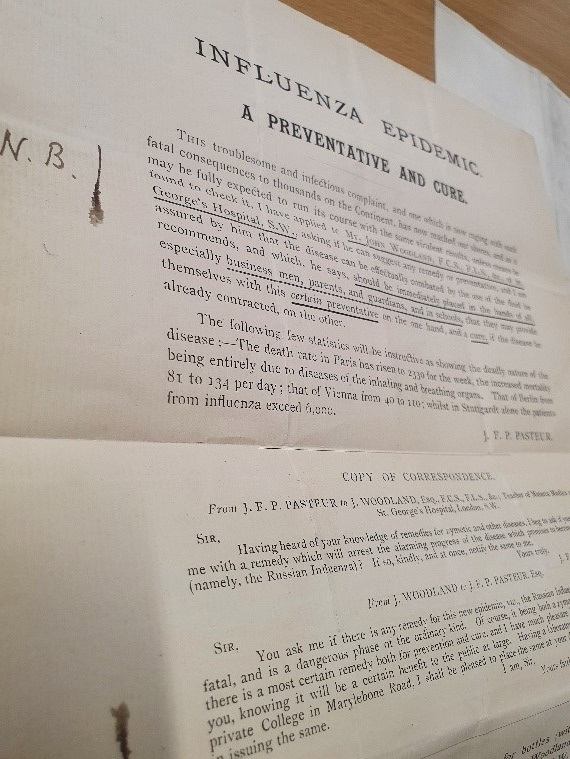 ‘Woodland affaire’, 1890. Archives and Special Collections, St George’s, University of London.
‘Woodland affaire’, 1890. Archives and Special Collections, St George’s, University of London.
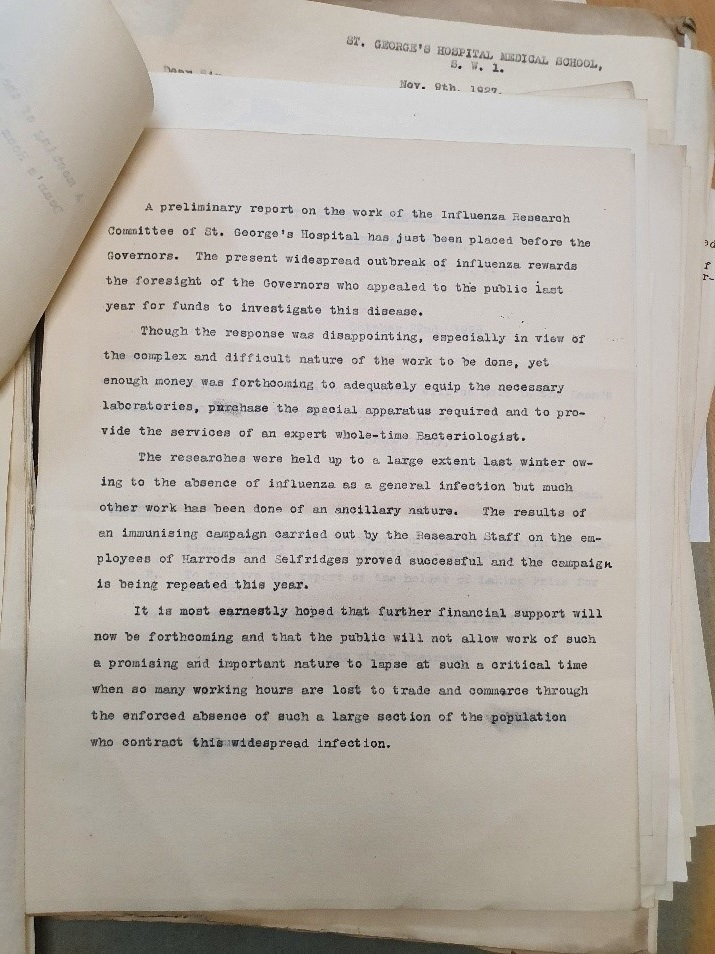
Influenza also continued to be a concern even after the 1918-1919 pandemic had abated, and in the 1926 St George’s decided to get involved in researching vaccines for influenza. There was a public funding campaign for the project, and in February 1927, St George’s published a letter in The Times:
‘following on the traditions established here by Jenner and Hunter in their historical work, we are […] engaged in special research with the object of ascertaining what causes influenza, how it can be controlled, how it can be prevented from spreading and, finally, whether a really effective treatment can be found for it’.
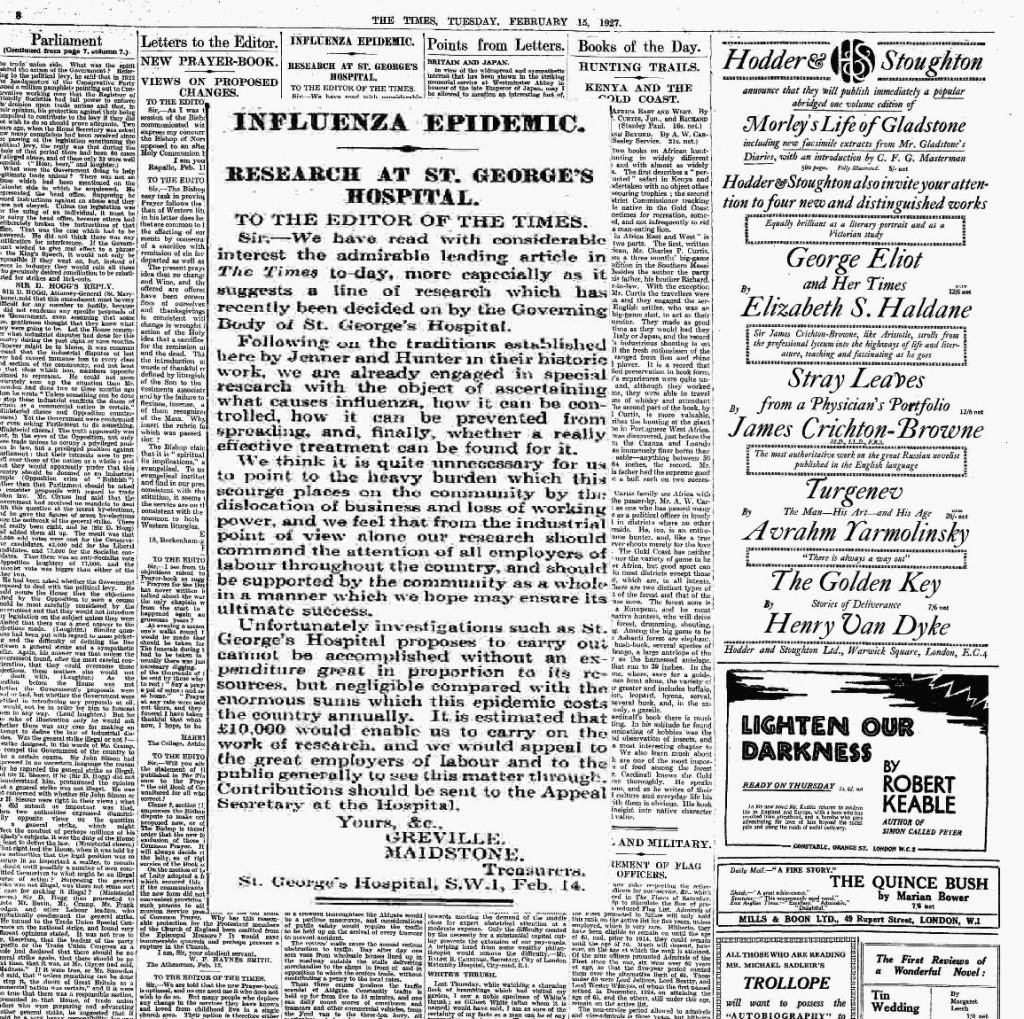 ‘Influenza epidemic: Research at St George’s Hospital’. The Times, 15 Feb 1927.
‘Influenza epidemic: Research at St George’s Hospital’. The Times, 15 Feb 1927.
The arguments found in the plea for funding sound familiar: the ‘heavy burden which this scourge places on the community by the dislocation of business and loss of working power’. Because the project was widely publicised, the public was eager to take part, and we have some wonderful letters from people writing in and suggesting their own cures and theories of the causes of influenza: we will be tweeting these, so look out for them on our Twitter feed!
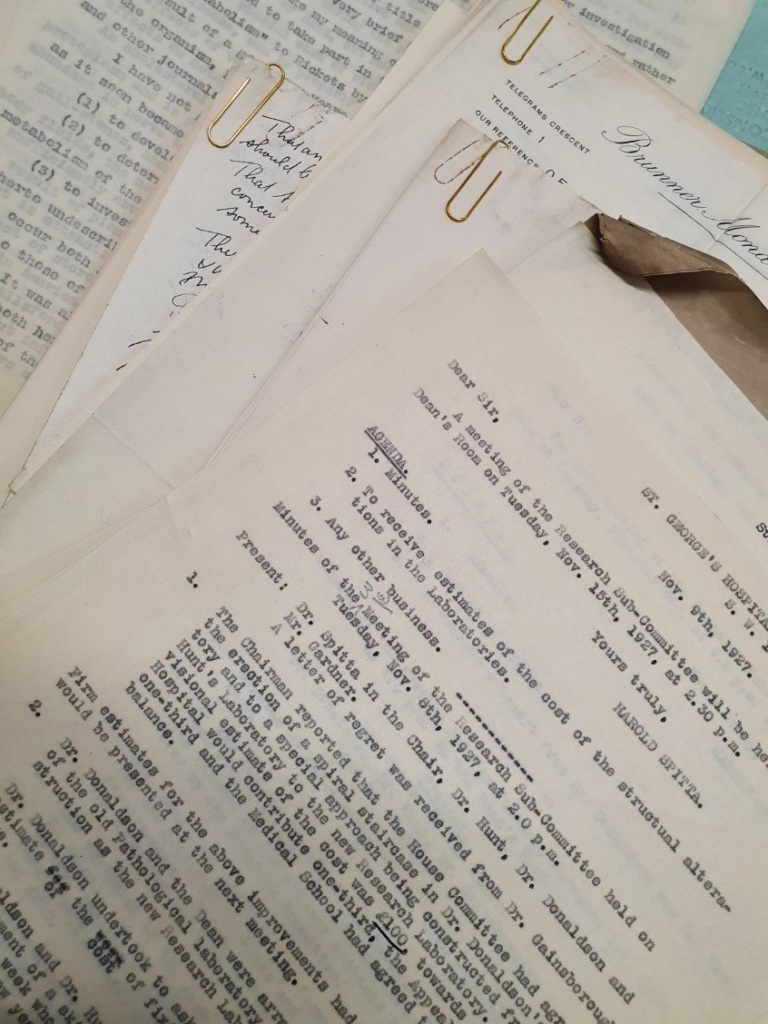 Records relating to influenza research. Archives and Special Collections, St George’s, University of London.
Records relating to influenza research. Archives and Special Collections, St George’s, University of London.
The money for the research was found, and the subject of the vaccinations was chosen to be the staff of Harrods and Selfridges on Oxford Street, as well as the staff at Quin & Axtens and Bon Marché in Brixton, department stores which had recently been acquired by Selfridges. Altogether 345 people were vaccinated.
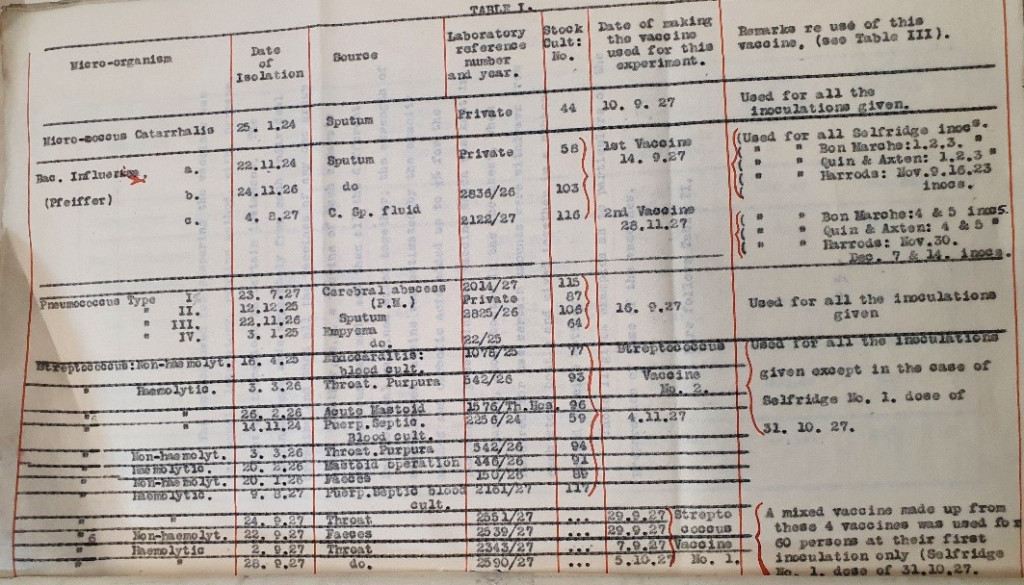 Table 1, ‘Report on anti-catarrh inoculations (catarrh of respiratory mucous membranes)’, 1928. Archives and Special Collections, St George’s, University of London.
Table 1, ‘Report on anti-catarrh inoculations (catarrh of respiratory mucous membranes)’, 1928. Archives and Special Collections, St George’s, University of London.
The various reports, meetings minutes and correspondence held in the archives tell us how the research subject was decided on, issues to do with the research, space and equipment (including the building of a spiral staircase in the laboratory – obviously an essential architectural refinement) and, most importantly, how the research was conducted and what the results were.
The report of the findings in 1928 shows the research was conducted using attenuated vaccine ‘obtained from pathological fluids or secretions or from a mucous surface of persons who exhibited clinical evidence of disease’, with the assumption that the disease was called by a bacterium called Pfeiffer’s bacillus, or Haemophilus influenzae (also known as h-flu). It was not until a few years later, in 1933, that it was definitely established that influenza was actually viral, and not bacterial.
And the results? Well, it appears that 1927 was a disappointing year when it comes to influenza, at least from the researchers’ point of view. The vaccination campaign was, however, declared a success, and there were plans to repeat it the following winter (although if that did happen, the records have not survived).
 Response to ‘Report on the work carried out in the Research Laboratory’, 11 Jul 1928. Archives and Special Collections, St George’s, University of London.
Response to ‘Report on the work carried out in the Research Laboratory’, 11 Jul 1928. Archives and Special Collections, St George’s, University of London.
The preserved documents reveal an on-going preoccupation with and interest in influenza, even though (given what we are currently going through) there does not appear to be much sense of urgency, certainly not at the time of the 1918 influenza.
Although the research was not successful in finding a vaccine that worked, it was an important step on the way: you won’t know what works until you try it. Our knowledge is cumulative, and dead-ends are part of research – not everything can work out, but it all adds up. The first influenza vaccine was developed in the 1940s, and (soon, hopefully) we will see a COVID-19 vaccine.
Looking forward
What does this all have to do with digital preservation, then? Compared to the 1918 and 1889 flu pandemics the records we are creating today are largely digital. The technology supporting these records change rapidly and may one day become obsolete. If this happens, we could lose access to valuable records, including our covid-19 records. St George’s has recognised this and is actively engaged in looking after our digital information for the long term. We’ve recently purchased a digital preservation system, Preservica, to help us to preserve our digital records. We are working to develop methods and processes that will allow us to preserve the records that are currently being created, and to do so in a meaningful way that will work for colleagues across the organisation.
Rather than thinking of digital and physical something entirely separate, we should consider them as part of a continuum, as it were. Preserving digital material can be challenging, and we can’t always replicate the processes used for paper with digital material, but the gaps in the past records show the need to preserve evidence of the current pandemic, not only for historical interest but to provide evidence of what happened and how we dealt with it.