This article is part of a series of research impact stories related to our REF 2014 submission.
Professor Nidhi Sofat credits the symbiosis between City St George’s and St Georges University Hospitals NHS foundation trust for helping her uncover the secrets of osteoarthritis, pointing towards new diagnostic tools and drug development.
The joint condition osteoarthritis causes chronic pain and misery for millions of people in the UK. Right now, the best option for patients is to rely on pain killers until their condition gets so bad that they need a joint replacement. There are currently no treatments that halt the progression of osteoarthritis, partly because the underlying biological drivers of the disease are not well understood.
Osteoarthritis is the most common form of arthritis, affecting more than 8.75 million people in the UK
‘Cartilage gets damaged as one of the early steps in osteoarthritis, followed by changes in the underlying bone’ says City St George’s consultant rheumatologist Professor Nidhi Sofat. Until recently, these changes in the bone, known as bone marrow lesions, were just mysterious shadows on MRI scans. Doctors knew they caused patients significant pain, but they didn’t really know what they were or how to treat them.
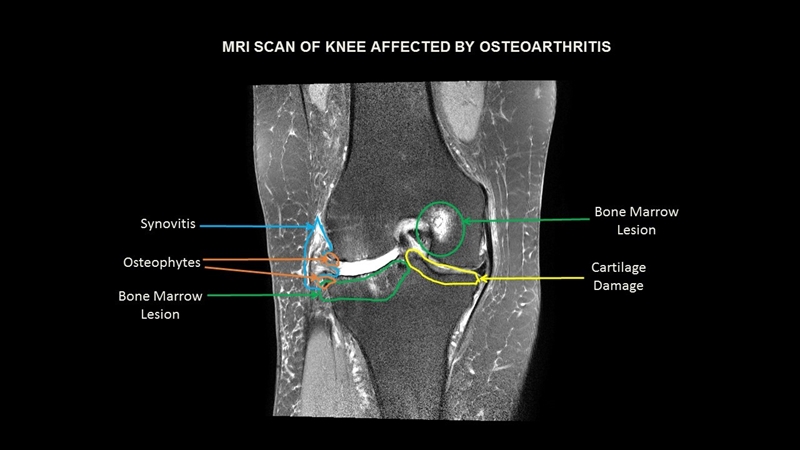 An MRI scan of a knee affected by osteoarthritis.
An MRI scan of a knee affected by osteoarthritis.
In a study supported by the Rosetrees Trust and the National Institute for Health Research, Sofat and her team studied samples of bone marrow lesions from the knee joints of people with osteoarthritis. ‘We saw more blood vessels and more nerves in these lesions, which might explain why the patients are experiencing so much pain,’ says Sofat. The team also found that genes involved in forming new nerves and blood vessels were more active in the bone marrow lesions, compared with healthy tissue.
Sofat explains that the partnership between the university and the NHS foundation trust was essential for her research. Splitting her time between treating patients and conducting research enabled her to understand not only the molecular drivers of osteoarthritis but also its impact on patients, and helped with recruiting participants for her studies.
 Professor Nidhi Sofat working with a patient.
Professor Nidhi Sofat working with a patient.
So, what’s next? ‘We’re now testing whether the products of these genes could be useful as biomarkers to diagnose osteoarthritis,’ she says. ‘We hope they will give us some clues as to which pathways are affected in this condition and help us understand what to target for treatments in the future.’