By Natasha Shillingford. This text was originally published as 'The Post Mortem Examinations and Case Books as a Source for Genealogical Research', St George's Library Blog, 25 Feb 2021.
Previous blog posts have highlighted the value of the Post Mortem collection for contributing to our understanding of medical education, death practices, and the history of London’s hospitals and infectious diseases. However, it is also a valuable and rich resource for genealogy and tracing your family history. The collection consists of 76 volumes, and an estimated total of 36,000 cases which is a lot of names! The majority of the patients admitted to St George’s Hospital were from the lower classes as wealthier individuals were able to pay physicians to attend to them in their homes. Therefore, the Post Mortem Examinations and Case Books provide information about working class patients who may not be represented in many other records and can provide additional or missing information about your ancestors.
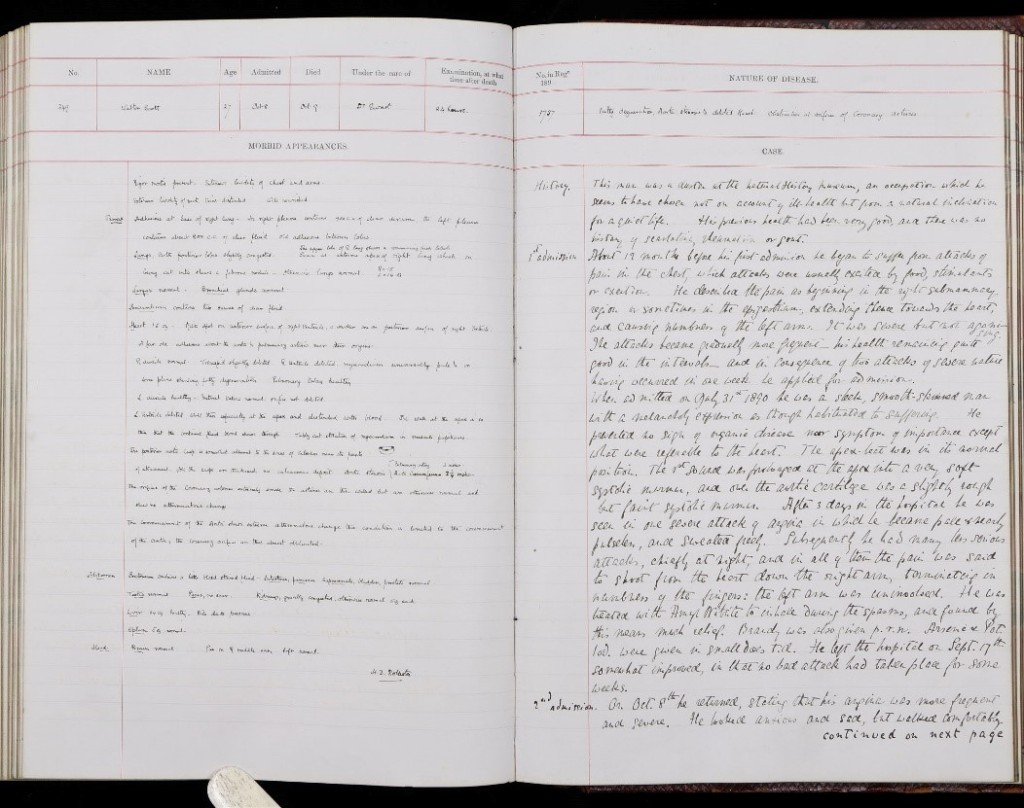 PM/1890/349. Archives and Special Collections, St George’s, University of London
PM/1890/349. Archives and Special Collections, St George’s, University of London
The right-hand page is reserved for details of the medical case before the patient’s death. It records the patient’s medical history, current symptoms which caused them to attend the hospital, a description of the patient on admission and details of the treatments prescribed and changes in condition prior to their death. On first glance the medical case history appears to be rather formulaic but on closer inspection they provide fascinating insights into the patients and provide a glimpse into their life before death.
From 1st July 1837 all births and deaths had to be reported to a local registrar, who in turn reported them to the superintendent registrar of the registration district where the birth or death occurred. Since 1874 doctors’ certificates were also required by a registrar before a death certificate could be issued. A death certificate records where and when the individual died, name and surname, sex, age, occupation, cause of death, the signature, description and residence of the informant, when the death was registered and the signature of the registrar.
The death certificate of George Danbury will undoubtedly list his death simply as Tetanus. However, the medical notes expand on this diagnosis and tell us that ‘A fortnight before his admission George Danbury ran a nail into the ball of his right great toe. He felt no pain but later felt stiffness of the jaw and pain in the back. On admission he could not open his jaw and there was stiffness and pain in the back of the neck. He began to experience spasms, had a good deal of sweating and the head became retracted and fixed.’ (PM/1870/258)
The case notes often include the medical history of other family members to determine if the patient could be suffering from an inheritable disease. This is invaluable for tracing other family members of the deceased. Fifty-three-year-old Henry Moon died in 1889 from ‘Carcinomatous stricture of Oesophagus’. The case notes begin ‘The patient was a clerk. He gave a family history of carcinoma. One aunt had died of cancer of the throat, another of cancer of the stomach, a cousin of cancer of the eye.’ (PM/1889/285). The medical case notes will also record if they came from a phthisical (tuberculous) family, and if their parents lived to an old age. If the patient is female, it will often be noted how long they had been married, how many children they had given birth to, how many children were living at the time of her admission, and how many miscarriages the woman had suffered. The case notes for Sarah Harris records ‘Pregnancies = 9. Children = 8. Miscarriage = 1, in Dec last at 5 months. Says that during this last pregnancy had ‘fits’ when about 4 ½ months gone, from which time till she aborted she did not feel the child. A doubtful abortion in Feb last.’ (PM/1881/388). Ellen Pointon, a thirty-nine-year-old Widow ‘had been married for 9 years. She had had 1 miscarriage and four children, 3 of whom were alive when she came into the hospital.’ (PM/1888/301)
The case notes often track a patient’s travel both within the UK and abroad to determine the origin of the disease, particularly if the disease is highly infectious. Amy Bradshaw, a seven-year-old girl, was admitted to St George’s Hospital on 24th July 1883 and she later died on 10th January 1884. She was suffering from Leprosy. The medical case notes record that ‘Her mother was a native of Oxfordshire, her father of Barbados, where his family had lived for three generations since leaving Scotland.’ Amy was one of six children, one of whom died in infancy of Dysentery, and two had Leprosy. The sister next above her in age was four and a half years older, and she developed symptoms of Leprosy in 1875 (PM/1884/9). Charles Dilloway was a footman who had just returned from a foreign tour. Twenty days before his admission he was in Rome. He returned via San Remo, Cannes and Boulogne. ‘He was back in England a fortnight before he came to the hospital. After his return he lived at 35 Chesham Place Belgrave Square’ where he slept below ground. Not only is each city he travelled through recorded in the case notes, the physician has also recorded the name of each hotel that he stayed at during his travel back to England.
Furthermore, the physicians often record the address of the patient along with living conditions if they believe it is relevant to the disease, such as in the case of a four-year-old boy called Albert Pratt. His ‘Parents lived at Brighton but the child had been staying at 1A Bulmer Place Notting Hill Gate. In this house the floor of the W.C. [Water Closet] was in a very bad state, having all crumbled away. The Landlord refusing to do anything. Within the last 6 weeks 6 persons living in the house, 4 children and 2 young women had had sore throats but all recovered.’ Young Albert, was diagnosed with Diphtheria and ultimately succumbed to the illness. (PM/1889/22)
Diet is often commented on in the medical case notes, such as in this case of 15 year old John Landeg who died of Scurvy in 1882. ‘When admitted the boy stated that he had been feeling weak and ill for four or five months previously. That he had a dislike to [non] salt meat and consequently had for the last four or five weeks been eating only salted meat. He was an office boy, in the habit of taking away from home meat for the whole day, and consequently rarely eat vegetables. Got potatoes on Sundays only.’ (PM/1882/366)
Alcohol consumption is also often recorded, such as in the case of 25 year old Alfred Balcombe who was described as ‘A coachman of intemperate habits, a beer drinker, reported to be generally in a fuddled state, refusing his food and supplying its place with beer, ’ (PM/1866/18) or Frederick Osborne, a forty five year old labourer, who had ‘always been accustomed to drink beer, avoiding the weaker kinds and drinking chiefly ‘six ale,’ and some spirits. The average quantity of beer was five or six pints daily.’ (PM/1888/95)
Occupations are listed where known, and the medical case notes often expand on simple terms such as ‘Groom’ or ‘Soldier’. Elbra Appleby died in 1881, aged fifty-one. In his work as a painter he had been exposed to so much lead that, despite precautions, he developed colic and wrist drop, losing strength in both hands and becoming irritable and depressed (PM/1881/392). John Lewicki was ‘An old soldier, formerly on Napoleon’s Polish lancers. He had fought in nearly all the wars of the empire. He had been frost-bitten at Beresina, and again at Moscow. He was wounded at Austerlitz, recovered a sabre cut at Vittoria. Altogether he shewed seven scars. He escaped from Waterloo unhurt. Latterly he enjoyed a pension for a few years, but lost it on account of his republican views. He was expelled from Paris and contrived to get his living by selling pencils about the streets of London. He attributed his illness to eating sprats.’ (PM/1860/36)
Sometimes the comments of the physicians can be extremely evocative and paint a picture of the patient on their admission. For example, the doctor Octavius Sturges (1883-1894) describes various patients as ‘an anxious, delicate girl with an anxious, sad expression’, another as a ‘dark, spare person of melancholy aspect, a needlewoman’, another as ‘stout and well-built with the countenance of a drunkard’ or ‘a miserable, emaciated old man having the withered and wrinkled face of a mummy’.
The case notes sometimes include anatomical sketches and drawings, and occasionally portraits of the patient, such as in the case of Thomas Roles, a 49-year-old Shopkeeper, who was admitted to St George’s with a tumour of the face which was removed by operation.
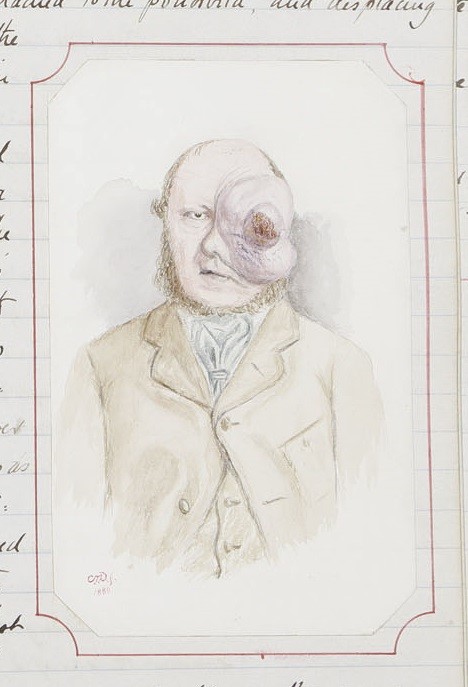
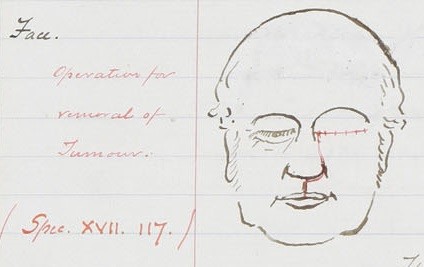
PM/1880/236. Archives and Special Collections, St George’s, University of London
The left-hand page, labelled ‘Morbid appearances’, is used to record the details in the post mortem examination, with each part of the body examined in depth. The morbid appearances also include a general description of the body, recording information such as height, weight and hair colour. At a time when photography was unusual for many working-class Londoners such as those attending St George’s Hospital, the general description at least provides a hint as to their appearance. Thomas Roles was described as ‘Well nourished. Obese. 5’6” high. Hair dark.’
In conclusion, the Post Mortem Examinations and Case Books are a unique and fantastic resource for tracing the lives of working-class individuals in London, and the information provided in the volumes almost serves to bring the patients back to life.